Introduction
A 20-year-old man was admitted to our department with complaints of swelling and pain in the left mandibular region. Although he had undergone several surgical procedures over 12 years, the condition remained unresolved. Extraoral examination showed facial asymmetry resulting from a widening of the left mandibular angle (Fig. 1). Axial computed tomography (CT) scans revealed a radiolucent lesion causing cortical expansion on the left side of the mandible (Fig. 2a), and 3-dimensional CT scans showed severe facial asymmetry caused by the expansile lesion (Fig. 2b).
On intraoral examination, deep carious lesions and adjacent gingival inflammation were found in the lower first and second molars, which were painful to percussion. The regional submandibular lymph nodes were enlarged, tender and mobile. There was no fluctuant swelling, drainage or fistula and no evidence of periapical pathology.
Lower first and second molars were extracted and an incisional biopsy was performed. Follow-ups confirmed complete healing of the extracted sockets; however, there was no sign of regression of the extraoral swelling. After a provisional diagnosis was made, the lesion was completely removed.
 Figure 1: Extraoral photograph revealing swelling over the lower border of the mandible on the left side.
Figure 1: Extraoral photograph revealing swelling over the lower border of the mandible on the left side.
 Figure 2: Axial computed tomography scan showing a radiolucent lesion causing cortical expansion on the left side of the mandible (a), and 3D scan revealing severe facial asymmetry (b).
Figure 2: Axial computed tomography scan showing a radiolucent lesion causing cortical expansion on the left side of the mandible (a), and 3D scan revealing severe facial asymmetry (b).
What is your diagnosis?
Differential Diagnosis
The differential diagnosis included Garré's osteomyelitis, fibrous dysplasia and chronic diffuse sclerosing osteomyelitis.
Garré's Osteomyelitis
Garré's osteomyelitis or proliferative periostitis is a type of chronic osteomyelitis that is nonsuppurative and primarily affects children and adolescents.1 It commonly occurs in young patients with a mean age of 13 years,2 although sporadic cases have been reported in 20–65 year olds.3
The mandible is the most commonly affected area in the maxillofacial region. The process arises secondary to a low-grade chronic infection, usually from the apex of a carious mandibular first molar. The infection spreads toward the surface of the bone, resulting in inflammation of the periosteum and deposition of new bone under the periosteum. This peripheral formation of reactive bone results in localized periosteal thickening. The inferior border of the mandible below the carious first molar is the most common site for hard nontender expansion of cortical bone.
Fibrous Dysplasia
Fibrous dysplasia of bone is a skeletal disorder characterized by extensive proliferation of fibrous tissue in bone marrow, leading to osteolytic lesions, fractures and deformations. Initial symptoms most often appear during childhood or adolescence as bone pain and repeated fractures. Other usual clinical findings are bone deformity and neurologic compression, especially when the facial bones or the skull are involved.
Radiologic signs of fibrous dysplasia consist mainly of lytic and cystic lesions, reduction of cortical thickness and, sometimes, widening of the diaphysis.
The radiographic appearance of fibrous dysplasia varies with maturation of the lesion; opacity generally increases with maturity. The generally younger age of onset and its unilateral distribution helps to differentiate fibrous dysplagia from Paget's disease, which affects older patients and is frequently bilateral.
Chronic Diffuse Sclerosing Osteomyelitis
Diffuse sclerosing osteomyelitis of the maxilla or mandible is characterized by recurrent pain and swelling, often associated with trismus. It is associated with organisms of low virulence, and its etiology is poorly defined. Bacterial infection has been suggested as a cause, but antimicrobial treatment is usually unsuccessful. Chronic periodontal disease, which appears to provide a point of entry for bacteria, is important in the etiology and progression of diffuse sclerosing osteomyelitis. Carious nonvital teeth are not usually implicated.
This condition may be seen at any age, in either sex and in any race, but it tends to occur most often in middle-aged black women.
Radiographically, the lesions show variable amounts of deposition of bone and diffuse sclerosis with ill-defined borders.5
Treatment
Histopathologic examination of the biopsy specimen suggested chronic osteomyelitis. The patient was operated on under general anesthesia via oroendotracheal intubation. An intraoral incision extending from the lower left second premolar to the ascending ramus of the mandible was made, a mucoperiostal flap was elevated and the lesion was curetted and removed. A final histopathologic evaluation revealed fibrous alterations of the bone marrow, chronic inflammatory cell infiltration and irregularly shaped reactive bone areas (Fig. 3). The final diagnosis was chronic diffuse sclerosing osteomyelitis.
At a 6-month follow-up assessment, a reduction in the size of the swelling was detected (Fig. 4).
 Figure 3: Histopathologic examination revealed fibrous alterations of the bone marrow (a), chronic inflammatory cell infiltration (b), and irregularly shaped reactive bone areas (c). Hematoxylin and eosin staining, magnification × 40.
Figure 3: Histopathologic examination revealed fibrous alterations of the bone marrow (a), chronic inflammatory cell infiltration (b), and irregularly shaped reactive bone areas (c). Hematoxylin and eosin staining, magnification × 40.
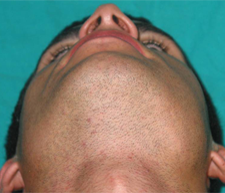 Figure 4: Extraoral photograph showing recession of hard swelling on left side.
Figure 4: Extraoral photograph showing recession of hard swelling on left side.
THE AUTHORS
References
- Oulis C, Berdousis E, Vadiakas G, Goumenos G. Garre's osteomyelitis of an unusual origin in a 8-year-old child. A case report. Int J Paediatr Dent. 2000;10(3):240-4.
- Eswar N. Garre's osteomyelitis: a case report. J Indian Soc Pedod Prev Dent. 2001;19(4):157-9.
- Martin-Granizo R, Garcia-Gonzalez D, Sastre J, Diaz FJ. Mandibular sclerosing osteomyelitis of Garré. Otolaryngol Head Neck Surg. 1999;121(6):828-9.
- Singer SR, Mupparapu M, Rinaggio J. Clinical and radiographic features of chronic monostotic fibrous dysplasia of the mandible. J Can Dent Assoc. 2004;70(8):548–52.
- Jones J, Amess TR, Robinson PD. Treatment of chronic sclerosing osteomyelitis of the mandible with calcitonin: a report of two cases. Br J Oral Maxillofac Surg. 2005;43(2):173-6.
