ABSTRACT
Background and Objective: The types of cancers that most frequently metastasize to the mouth and jaws reflect, for the most part, the relative incidence of cancers in a given population at a given time. We report a retrospective, but relatively contemporary study of 38 cases of metastatic oral tumours in a Canadian population to compare the Canadian experience with that of nearby and distant countries.
Methods: Thirty-eight cases of metastatic disease to the mouth and jaws in a Canadian population were analyzed. Data about patients' age, sex, site of metastatic deposits, clinical history, including the presence of a known primary cancer, and radiographic features were collected from the files (1992–2010) of the oral pathology diagnostic service at the University of Western Ontario, and the hospital archives (2002–2010) of the department of pathology, London Health Sciences Centre, London, Ontario.
Results: Most metastases were to the mandible, although oral soft tissues were also involved, most frequently, the gingiva and mucosa of the alveolar ridge. Prostate, lung and breast cancers were the most common primary sites, but a variety of cancer types were found.
Conclusions: The relative frequency of types of metastatic cancer to the oral region is similar in Canada, the United States and Northern Europe, but differs significantly from those reported in South East Asia and Japan. The relative frequency of types of cancer that metastasize to the mouth and jaws reflects the relative incidence of cancers in the population.
Introduction
Carcinomas are the most common types of cancers that metastasize to the mouth and jaws.1,2 Although the oral soft tissues may be affected, particularly the gingiva and mucosa of the alveolar ridge, and the tongue, metastases to the jaw bones, especially the posterior mandible, are considerably more common.1,2 Metastatic disease may be multifocal in these tissues. The actual incidence of these cancers is unknown since oral metastatic disease is usually a manifestation of advanced disease and an unknown number of patients die without investigation for occult oral metastases. Even if an autopsy is done, the mouth and jaws are not commonly examined because family and undertakers often object to the resulting facial mutilation. Known cases involve patients who develop symptomatic oral metastases while they are still alive. Metastatic foci from distant sites in the abdomen or thorax are thought to be deposited by the blood vascular system, largely through Batson's vertebral and paravertebral plexus of veins, or by tertiary deposits from metastatic lung foci.3 Oral metastasis carries a grave prognosis for the patient because it represents advanced disease. Affected patients usually die within a year.4,5
Most reports of oral metastases involve 1 or 2 case reports from scattered geographical areas, or reviews of these reported cases,1,2,5 but surprisingly, few series of oral metastatic disease from a given geographic region are reported. Some of these series are small and outdated6,7 and because of changes in the incidence and mortality of cancer types over time in a population,8 they are not useful for a contemporary comparison of data. Even more recently published series from the United States9,10 and Europe,11 and a review of the Japanese literature12 include cases from distant decades that skew their data because of contemporary shifts in the incidence of various cancers.8 The series reported by Lim and colleagues13 from Korea is relatively more contemporary. Nevertheless, comparison of the data reported from these geographic regions show significant geographic variation in the frequency of the types of tumours that metastasize to the mouth and jaws. Because we were unable to find a previous report of a series of metastatic tumours to the oral region in a Canadian population, we report a retrospective, but relatively contemporary study of 38 Canadian cases, and compare this Canadian experience with that of nearby and distant countries.
Methods
The files of the oral pathology diagnostic service at the University of Western Ontario, London, Ontario, which receives specimens from dentists and dental specialists from across the province of Ontario, were searched for cases of metastatic tumours to the jaws and oral soft tissues occurring between 1992 and 2010. All tissue sections, reports and any related materials were retrieved and examined. Additional cases were retrieved from the hospital archives of the department of pathology, London Health Sciences Centre, London, Ontario, for the years 2002 to 2010. Data about patients' age, sex, site of metastatic deposits, clinical history, including the presence of a known primary cancer, and radiographic features were collected from information submitted on biopsy requisition forms by the clinicians who took the biopsies, and from examination of radiographs if these were also submitted with biopsied tissues. Previously reported lymphomas14 were not considered metastatic and were excluded.
Results
Table 1 summarizes the 38 cases of neoplasms that metastasized to the mouth and jaws, and patients' sex, age and sites of metastatic deposits. The mean age of patients was 69.6 ± 12.0 years (range 32.0–88.0 years; median 69.0 years); more than half (58%) of the 38 patients were men (22 men, 16 women). Data collected for these patients did not include their ethnic origin. However, the 2006 Canadian census showed that the population of Ontario was dominated by whites of European descent with over 200 reported ethnic origins. Of the visible minorities, 28.9% were South Asian, 21.0% Chinese, 17.3% black, 7.4% Filipino, 5.4% Latin American and 4.1% Arabic.15
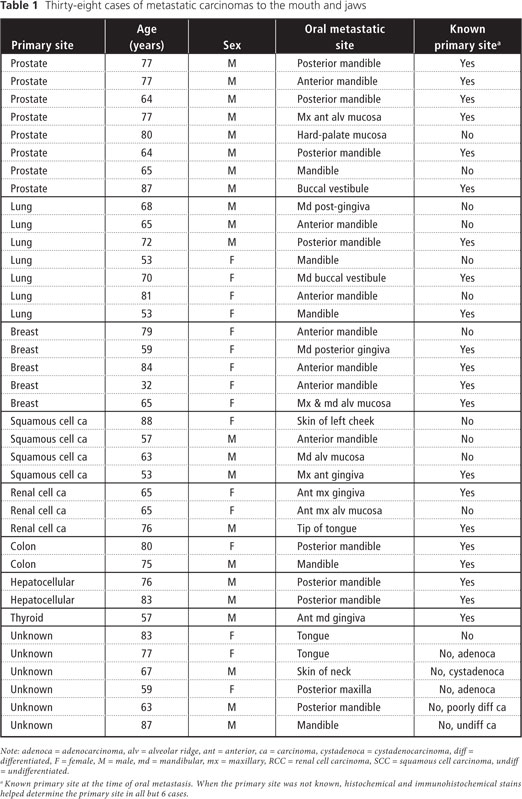
Twenty-one (55%) of the 38 patients had a known primary tumour at the time of oral metastasis; none had sarcomas. Patients over 60 years of age accounted for 30 (79%) of 38 oral metastases, and only 1 (3%) tumour occurred in a patient under 50 years of age. Figure 1 illustrates the frequency of tumours occurring at various ages, by decade. Twenty (53%) of the 38 neoplasms occurred in the mandible; the anterior mandible was affected in 7 (35%) of these 20 cases (Fig. 2), and the posterior mandible in 8 (40%) cases; no distinction was made in the remaining 5 (25%) cases. Only 1 neoplasm, a poorly differentiated adenocarcinoma, occurred in the maxilla in the right molar area. Lesions mimicking periapical inflammatory lesions were found, although radiography showed that they were often multifocal (Fig. 3), suggesting possible metastatic tumour deposits. Maxillary lesions were more often found in the gingiva or edentulous alveolar mucosa (Fig. 4) than in bone. The maxillary gingiva and alveolar crest mucosa were affected 4 times, the mandibular gingiva and alveolar mucosa 4 times, the tongue 3 times, the buccal mucosa and facial skin 2 times each and the mucosa of the hard palate once. One neoplasm affected both the maxillary and mandibular alveolar mucosa.
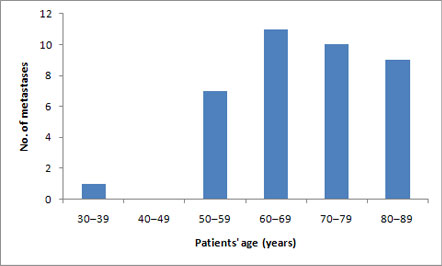 Figure 1: Number of metastatic cancers of the mouth and jaws occurring in study population (n = 38) by decade of patients' ages.
Figure 1: Number of metastatic cancers of the mouth and jaws occurring in study population (n = 38) by decade of patients' ages.
 Figure 2: This 64-year-old man had prostate carcinoma metastatic to the anterior mandible. There are multiple radiolucencies bilaterally, some of which mimic periapical disease.
Figure 2: This 64-year-old man had prostate carcinoma metastatic to the anterior mandible. There are multiple radiolucencies bilaterally, some of which mimic periapical disease.
 Figure 3: A 32-year-old woman had metastatic deposits of breast carcinoma at the apices of the mandibular molars that mimicked periapical inflammatory disease.
Figure 3: A 32-year-old woman had metastatic deposits of breast carcinoma at the apices of the mandibular molars that mimicked periapical inflammatory disease.
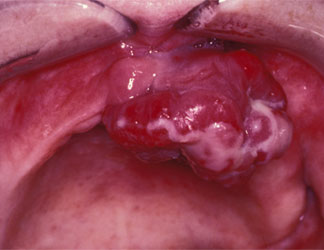 Figure 4: A 65-year-old woman had this rapidly growing, nodular metastatic renal cell carcinoma of the mucosa of the anterior maxillary alveolar ridge.
Figure 4: A 65-year-old woman had this rapidly growing, nodular metastatic renal cell carcinoma of the mucosa of the anterior maxillary alveolar ridge.
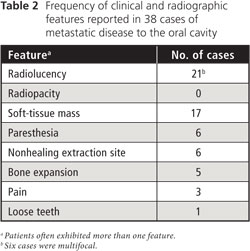
Clinical manifestations included pain, bony- or soft-tissue swelling, and loose teeth, but some lesions were asymptomatic. The most common clinical findings were paresthesia of the lower lip, which occurred in 6 (30%) of the 20 mandibular cases, a mass growing from a nonhealing extraction site (6 [16%] of 38 cases) and multifocal lesions (6 [16%] of 38 cases). Table 2 lists the frequency or reported clinical and radiographic findings of the 38 cases of metastatic cancers to the oral region.
The microscopic features of the tumours were diagnostic in some cases, but most required additional histochemical and immunohistochemical stains to determine the primary site. The primary site was unknown and could not be determined microscopically in 6 (16%) of the 38 cases. However, the determination of the primary site of these tumours could usually be narrowed with the use of the immunohistochemical markers that are common to specific groups of cancers and not found in others. For example, tumours of unknown origin from deep in the mandible were found to be adenocarcinomas, but, although it was possible to rule out the mandible as the primary site, it was not possible to identify a specific organ of origin microscopically. These patients would have required a clinical work-up for a differential diagnosis: some tumours are associated with elevated proteins in the blood, such as elevated prostate-specific antigen in prostate cancer, elevated hormone and enzyme levels in several types of cancer, M-component in plasma-cell myeloma, carcinoembryonic antigen in colonic cancer and breast cancer, and alpha-fetoprotein in hepatocellular carcinoma.16
Discussion
Metastatic disease to the mouth and jaws of patients from different geographical areas, including Canada, show similar clinical characteristics: soft- and hard-tissue swelling, pain, tooth mobility, bleeding and paresthesia. Radiographic characteristics of intrabony lesions were also similar: irregular, often multifocal radiolucencies, sometimes with fracture, or occasionally with increased opacity caused by aberrant tumour-induced bone formation by osteoblasts with cancers such as those of breast and prostate.9-13 In our series, a mass extruding from a nonhealing extraction site was also a common finding. As we found in our series, metastatic disease is generally accepted as a disease of the middle-aged and elderly. All series consistently show a significantly greater frequency of oral tumours in patients over 50 years of age,10-12 although scattered reports have involved younger people4,6,17 and children.3,14 Similarly, our data agree with those of reports that show oral metastatic disease tends to be cancers of the bone, especially the mandible.1,5,10 Most studies of oral metastatic disease indicate its predilection for the posterior mandible18 because of its rich blood supply in active areas of hematopoiesis. However, in our study, the anterior mandible was affected almost as often as the molar region. The gingiva or mucosa of the alveolar ridge is the most common soft-tissue site.2,5 The prevalence of oral metastatic disease in men and women varied, reflecting the type of cancers that most commonly metastasize to the mouth and jaws in a given population. Some studies showed a more or less even distribution between the sexes,10 whereas others showed more occurring in men12 or in women.13 In our study, the ratio of men to women was about 1.4:1.0, based largely on the high percentage of cases that were associated with a primary cancer of the prostate (8 of 38 cases).
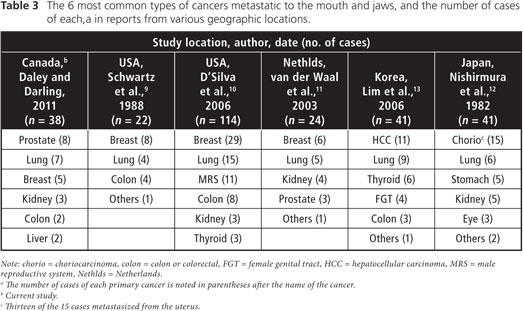
Despite the similarities in clinical and demographic data, significant temporal and geographic differences were found in the frequency of cancer types that metastasize to the oral region. Table 3 summarizes the frequency of various cancers from our series and reported series originating in the United States,9,10 the Netherlands,11 and Korea,13 and from a review of the Japanese literature.12
Although lung cancer is the most common cancer, when both male and female data are combined,8 it is not the most common metastatic lesion to the mouth and jaws in any geographic location, likely because oral metastases are a late feature, often of long-standing cancers. Further, most types of lung cancers result in rapid death, before oral metastases become clinically evident. Nevertheless, lung cancer is the second most common primary site in all geographic regions, including Canada, probably because of the widespread availability of tobacco products worldwide.
Significant differences in metastatic disease to the mouth and jaws occur among geographic regions. In our study of cases dating from 1992, we found that the prostate was the most common primary site (21%) for oral metastases in our Ontario study population. This finding is not surprising because in North America prostate carcinoma is estimated to be the second most common cancer (after lung and ahead of breast) since the major surge in incidence that occurred in 1988 and through the early 1990s.8 In 2006, D'Silva and colleagues10 from the United States reported that tumours of the male reproductive system, which they also called prostate carcinoma, were the third most common (10%), but their data were derived from cases that occurred as long ago as 1958, over 45 years ago. The large volume of pre-1988 cases masks the effect of the dramatic increase in the incidence of prostate carcinoma, which is greater than that of breast carcinoma, in the past 2 decades.8 Also supporting this notion are the findings of the 1988 US study of Schwartz and colleagues,9 based on data collected before the dramatic increase in incidence of prostate carcinoma. They reported only 1 example of prostate carcinoma and 8 examples of breast carcinoma in their 22 cases. Based on current evidence in our study done after 1988, we suspect that prostate carcinoma is, or will be, the most common metastatic lesion to the oral region in North America. In the Netherlands in 2003, van der Waal and colleagues11 reported 3 (12%) prostatic cancers in 24 cases, but like D'Silva and colleagues,10 much of their data predated the 1988 surge in prostate carcinoma reported for North America. However, their 12% relative frequency shows a trend to increased prostatic carcinoma metastases to the oral cavity, suggesting an increased incidence of prostate carcinoma in Northern Europe as well. In contrast to studies done in North America and Northern Europe, however, Nishimura and colleagues12 in Japan, and Lim and colleagues13 in Korea found no cases of prostate cancer as the primary site, even though they included contemporary data in their studies. In Japan, choriocarcinoma, which is more common in Japan than in North American or European countries, was by far the most common metastatic tumour to the oral region.13 Further, since Nishimura and colleagues' paper is a review of the Japanese literature, the rate of choriocarcinoma may be inflated by reporting bias, so its results cannot be easily extrapolated to other populations. We found no cases of choriocarcinoma metastatic to the oral region, nor were any reported in the American studies.9,10 In Korea, the most common metastatic tumour was hepatocellular carcinoma, reflecting its common incidence in Southeast Asia. Hepatocellular carcinoma is becoming a more common source of oral metastatic disease in North America and Europe because the incidence of hepatocellular carcinoma is increasing in these geographic regions.19
The actual incidence of metastatic disease to the oral region in Ontario is unknown, largely because of occult lesions, or undiagnosed known masses or radiolucencies present in the mouths and jaws of patients dying of terminal cancer. Studies such as ours cannot determine population incidence because dentists and dental specialists are the main source of our data; consequently, cases of oral metastatic disease diagnosed by physicians are not usually included. However, a strength of our study is the inclusion of cases derived from a hospital data source, including cases from both dental and medical personnel, that attempts to minimize, but does not remove this bias. Rather than population incidence, data from the current study show that the relative frequency of types of cancers that metastasize to the oral region reflects the incidence of these cancers in the North American population.
Additional series of metastatic diseases to the mouth and jaws from other geographic regions, including Africa and South America, are needed for a more complete global comparison.
Conclusions
This study shows that the relative frequency of metastatic disease to the mouth and jaws (namely, of the tissue of origin of the cancer) reflects contemporary trends and geographic variations in the incidence of cancers in a given population. This study shows that in Ontario, at this time, the most common cancers to metastasize to the oral cavity are those of the prostate, lung and breast.
THE AUTHORS
References
- Hirshberg A, Leibovich P, Buchner A. Metastatic tumors to the jawbones: analysis of 390 cases. J Oral Pathol Med. 1994;23(8):337-41.
- Hirshberg A, Leibovich P, Buchner A. Metastases to the oral mucosa: analysis of 157 cases. J Oral Pathol Med. 1993;22(9):385-90.
- Zachariades N, Koumoura F, Vairaktaris E, Mezitis M. Metastatic tumors to the jaws: a report of seven cases. J Oral Maxillofac Surg. 1989;47(9):991-6.
- Clausen F, Poulsen H. Metastatic carcinoma of the jaws. Acta Pathol Microbiol Scand. 1963;57:361-74.
- Zachariades N. Neoplasms metastatic to the mouth, jaws and surrounding tissues. J Craniomaxillofac Surg. 1989;17(6):283-90.
- Cash CD, Royer RQ, Dahlin DC. Metastatic tumors of the jaws. Oral Surg Oral Med Oral Pathol. 1961;14:897-905.
- Meyer I, Shklar G. Malignant tumors metastatic to mouth and jaws. Oral Surg Oral Med Oral Pathol. 1965;20:350-62.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71-96. Epub 2008 Feb 20.
- Schwartz ML, Baredes S, Mignogna FV. Metastatic disease to the mandible. Laryngoscope. 1988;98(3):270-3.
- D'Silva NJ, Summerlin DJ, Cordell KG, Abdelsayed RA, Tomich CE, Hanks CT, et al. Metastatic tumors in the jaws: a retrospective study of 114 cases. J Am Dent Assoc. 2006;137(12):1667-72.
- van der Waal RI, Butler J, van der Waal I. Oral metastases: report of 24 cases. Br J Oral Maxillofac Surg. 2003;41(1):3-6.
- Nishimura Y, Yakata H, Kawasaki T, Nakajima T. Metastatic tumours of the mouth and jaws. A review of the Japanese literature. J Maxillofac Surg. 1982;10(4):253-8.
- Lim SY, Kim SA, Ahn SG, Kim HK, Kim SG, Hwang HK, et al. Metastatic tumours to the jaws and oral soft tissues: a retrospective analysis of 41 Korean patients. Int J Oral Maxillofac Surg. 2006;35(5):412-5. Epub 2006 Feb 13.
- Daley TD, Yu J, Darling MR, Rizkalla K. Oral extranodal lymphoproliferative disorders of B-cell and T-cell origin. Can J Pathol. 2010;2(1):23-9.
- Government of Ontario, Ministry of Finance, Office of Economic Policy Labour and Demographic Analysis Branch. 2006 Census Highlights, Fact Sheet 11. April 30, 2008. Available: www.ontla.on.ca/library/repository/mon/22000/282039.pdf (accessed 2011 May 17).
- Rubin E, Rubin R, Aaronson S. Neoplasia. In: Rubin E, Gorstein F, Rubin R, Schwarting R, Strayer D, editors. Rubin's pathology: clinicopathologic foundations of medicine, 4th ed. Baltimore: Lippincott Williams & Wilkins; 2005. p. 165-213.
- Hatziotis JC, Constantinidou H, Papanayotou PH. Metastatic tumors of the oral soft tissues. Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol. 1973;36(4):544-50.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Metastatic tumours to the oral cavity — pathogenesis and analysis of 673 cases. Oral Oncol. 2008;44(8):743-52. Epub 2007 Dec 3.
- Daley TD, Minett CP, Driman DK, Darling MR. Oral metastatic hepatocellular carcinoma: a changing demographic in Europe and North America. Immunohistochemical advances in the microscopic diagnosis. Oral Oncol. 2011;47(1):62-7. Epub 2010 Aug. 21.
