Abstract
Objective: To conduct an observational, cross-sectional survey of the oral health status of adults ≥ 45 years of age in rural and urban long-term care (LTC) facilities in Nova Scotia, Canada.
Methods: Residents capable of informed consent were recruited by LTC staff in a stratified random sample of LTC facilities. Calibrated personnel administered standard clinical and quality-of-life instruments.
Results: Of the 335 adults (74% female) surveyed (mean age 80.8 ± 11.6 years), only 25% reported having regular dental care. Although 76% described their oral health as good or excellent, 41% were edentulous, 41% had some mucosal abnormality, 36% reported xerostomia and 25% had perceived or self-reported untreated dental conditions. Most mandibular dentures were nonretentive (59%) and almost half were unstable (49%). Among the dentate, 51% had untreated coronal caries, 44% had untreated root caries and 67% had attachment loss of ≥ 4 mm at ≥ 1 site. Predictors of coronal decay were a debris score ≥ 2 (adjusted odds ratio [adj OR] = 2.12; p = 0.045) or a history of smoking (adj OR = 1.02 per year of smoking; p = 0.024). Predictors of root caries were participants' perceiving a need for dental treatment (adj OR = 2.56; p = 0.015) or a history of smoking (adj OR = 1.02 per year of smoking; p = 0.026).
Conclusions: This epidemiologic study of the oral health of LTC residents revealed a high prevalence of untreated oral disease and low use of oral care services, highlighting the need for better access to oral care for this population.
Introduction
Canadians today are living longer1 and retaining more of their natural teeth2 than previous generations, emphasizing the need for a greater understanding of oral health over their lifespan. Seniors are a vulnerable population because they have limited access to oral health care; even more vulnerable are those living in long-term care (LTC) facilities. Research has consistently indicated that the oral health status of residents of LTC facilities is poor; the majority require some form of oral health care intervention.3
The percentage of teeth with decayed or filled root surfaces increases with each decade of adulthood, affecting more than one-half of all remaining teeth by age 75 years.4 For institutionalized elders especially, an increased risk for caries can be linked to inadequate daily oral hygiene, a high intake of refined carbohydrates and a propensity for xerostomia.5 The prevalence of xerostomia among institutionalized elders may be as high as 42%6 and is likely related to taking multiple medications,7 many of which reduce salivary flow.
Despite the high risk for oral diseases, this population faces greater barriers to receiving dental care than their independent counterparts.8 Among the reasons for limited access to oral health care are the inability of seniors to afford professional care and the lack of organized dental care for the institutionalized. In Canada, only in-hospital surgical-dental treatment is included in all provincial and territorial health insurance plans, whereas dental treatment is generally limited to programs for children or adults receiving income assistance.9 The passivity of the health system leaves the question of dental care entirely in the hands of senior citizens who are often limited by physical and organizational barriers (i.e., a lack of standards for oral health care delivery and provision of services) in LTC facilities.3
Obtaining clear, relevant data about the oral health status of residents of LTC facilities is an essential first step in planning strategies for the treatment and prevention of oral diseases in this setting. In this paper, we present the outcomes of a provincial survey of the oral health status of residents in LTC facilities in urban and rural Nova Scotia, and examine the predictors of oral disease in this population.
Methods
This study was part of an observational, cross-sectional survey of adults ≥ 45 years of age who were living in the community or in LTC facilities in Nova Scotia, Canada, in 2008–2009. We included in the study only those participants who were capable of giving informed consent. The consent emphasized that the survey was not a substitute for a regular dental examination. We received ethics approval from the Health Sciences Research Ethics Board at Dalhousie University and from District Health Authorities, when required.
Sample Size Determination
In 2006 there were 5827 beds in licensed LTC facilities in Nova Scotia.10 We used the known population prevalence rates of oral disease from an American survey11 of 5603 adults ≥ 40 years of age to determine the minimal sample size needed for this study. When we used the prevalence rate of periodontal disease for those ≥ 65 (53%) years of age, a confidence level of 95% and a finite population correction, we calculated that the minimal sample size required to estimate the prevalence with an error rate of 5% was 359 (6% of the population ≥ 65 of age in Nova Scotia).
Sample Selection
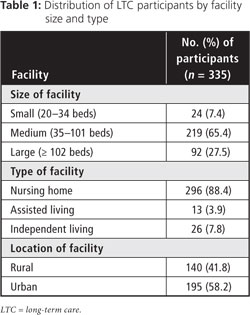
We included all private and government-owned LTC facilities in Nova Scotia with ≥ 20 beds per facility in our sampling frame (102 facilities). We chose the minimum bed capacity to facilitate efficient conduct of the survey. We assigned LTC facilities to either rural or urban strata, based on Statistics Canada's rural and small town definition of rural,12 and designated facilities as small (20–34 beds), medium (35–101 beds) or large (≥ 102 beds), based on capacity. Selecting a proportional sample within the rural and urban strata, we randomly sampled 39 facilities, 23 of which agreed to participate in our study. We recruited 7 additional facilities through a second random selection, and 1 urban facility volunteered (total = 15 rural and 16 urban facilities; Fig. 1).
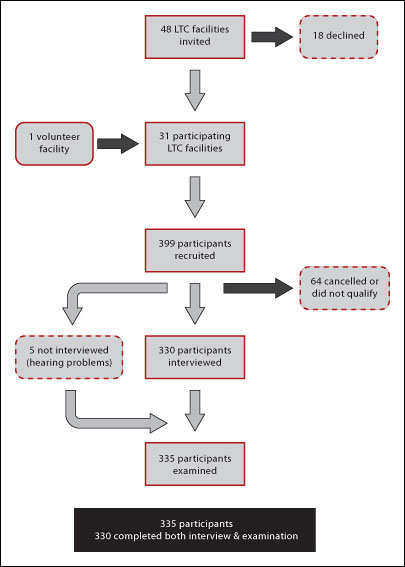 Figure 1: Sampling strategy. LTC = Long-term care.
Figure 1: Sampling strategy. LTC = Long-term care.
Questionnaire
A single trained interviewer, assisted by a francophone interviewer when required, administered a face-to-face questionnaire that measured the impact of oral health on quality of life, use of oral health care services and access to oral health care. Questions derived from the 2008 Canadian Health Measures Survey13 included demographics, use of dental care, perceived general health and oral health, regular oral hygiene habits, chronic health conditions, medication use, and history of smoking and alcohol consumption. Additional survey questions determined perceived need for dental care, reasons for not receiving regular dental care and amount paid for dental care. Oral Health-Related Quality of Life was assessed with the OHIP-1414 (data not reported here). We had the entire questionnaire translated into French and reviewed by an academic fluent in the local dialect.
Clinical Examination
Six calibrated dentists conducted intraoral examinations based on World Health Organization criteria modified for the Oral Health Module of the 2009 Canadian Health Measures Survey.15 We customized the survey by removing sections on fluorosis and orthodontic skeletal classifications, and adding an examination of jaw function and quality of prosthetics. The dentists examined participants in a portable A-dec chair (A-dec Inc., Newberg, OR) and an Aseptico light (Aseptico Inc., Woodinvile, WA) or in their wheelchair or bedside using a headlamp. The dentists took no radiographs.
The examining dentists recorded the degree of edentulism and reasons for loss of any teeth, excluding third molars, coronal and root caries, and type of restorative material in filled teeth. They determined periodontal and gingival status using the gingival index, debris index-simplified, calculus index-simplified, pocket-probing depth and clinical attachment levels. They assessed jaw function16 and recorded the stability, retention, hygiene and structural integrity of removable dentures.17
The dentists noted individual immediate and emergency treatment needs. Reasons for immediate treatment were asymptomatic untreated decay or periodontal disease, fractured teeth or dentures needing repair or replacement, and those for emergency treatment were pain, risk of cellulitis or suspected malignancy. In all cases, the dentists copied their recommendations to continue regular care, seek care at earliest convenience or seek care immediately to the care facility administrator. They did not recommend specific treatment.
Data Management and Analysis
A single research assistant entered all clinical data directly into a password-protected database. Two research assistants recorded data from interviews on paper and entered the data into the database. We ensured data quality with periodic quality control checks and interventions. We reviewed the clinical database weekly for missing or inconsistent data and reported any issues to the research assistant to anticipate and avoid future errors. For the interview data, each research assistant checked the other's data entry against the original hardcopy and corrected any errors.
We calculated logistic regression using PASW Statistics 17 (IBM SPSS Inc., Chicago, IL) to analyze predictors of denture use, coronal caries and root caries, and Poisson regression using Stata 9 (StataCorp LP, College Station, TX) to analyze predictors of the decayed, missing, filled teeth (DMFT) index. We used 2-tailed statistical tests and considered a p value ≤ 0.05 as significant.
Results
We conducted surveys in 31 LTC facilities in 21 communities from October to November 2008 and April to October 2009. Forty-two percent of participants resided in rural LTC facilities and 58% in urban facilities (Table 1), which is proportionate to the distribution of the general population in Nova Scotia. We recruited a total of 399 participants, out of which, 64 (16%) cancelled or did not qualify, and 330 (83%) completed both the interview and oral examination (5 in French, 225 in English); 5 (1%) people with hearing problems completed the clinical examination, but not the interview (Fig. 1). The survey sample was 93% (335/359) of the target sample.
Questionnaire
The average age of the participants was 80.8 ± 11.6 years (range 45.0–104.0 years; Table 2). More women than men participated in the survey, which reflects the gender imbalance in the Nova Scotia senior population.18
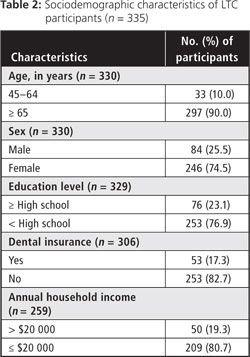
The median reported income range was CAD $10 000 to $20 000, lower than that of seniors living independently in the community. In 2006, the average income for households headed by someone between the ages of 65 and 74 years in Nova Scotia was CAD $44 371, and the income for households headed by someone ≥ 75 years of age was $36 858.1 Few (17%) participants had third-party insurance for dental care (Table 2).
More than half (52.8%) of participants were current (n = 29) or former (n = 148) smokers. The average number of years participants smoked was 34.2 ± 21.5 (range = 1–76).
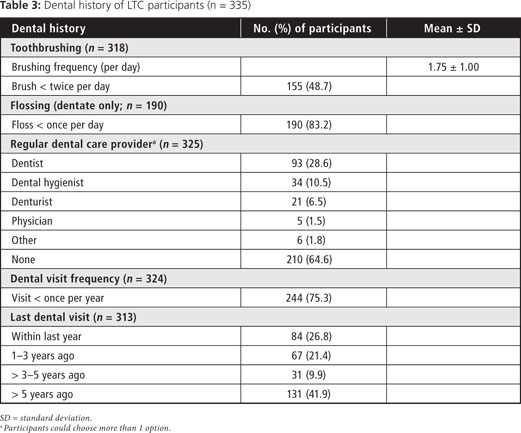
Most (75%) participants reported visiting a dental professional less than once per year and 42% reported their last visit to a dental professional was > 5 years ago (Table 3). Many (85%) reported having a chronic health condition and 98% were taking at least one type of medication. Despite this, two-thirds perceived their general health as good to excellent (Table 4). Similarly, although 53% reported dental or oral problems (xerostomia being the most common), only 25% thought they had untreated dental needs and about three-quarters perceived their oral health as good to excellent (Table 4).
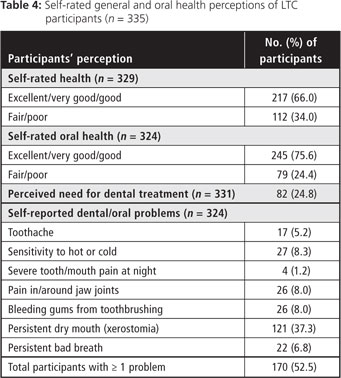
Clinical Examination
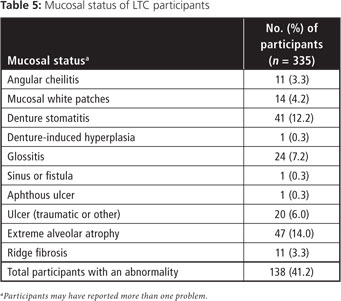
The average time to complete the oral examination was 12.3 ± 6.7 minutes (range 2.4–43.7 minutes, n = 335). Mucosal abnormalities were present in 41.2% of participants (Table 5). The most prevalent were related to edentulism: extreme alveolar ridge atrophy (14.0%) and denture stomatitis (12.2%). Glossitis was present in 7.2% and traumatic ulcers in 6.0% of the participants. The examining dentists found no lesions that suggested a possible malignancy during the survey.
Only 1 participant had significant occlusal wear, whereas 33.1% (n = 111) had inadequate occlusal contacts (i.e., occlusal contact between > 2 posterior teeth bilaterally). No participants had limited mandibular opening.
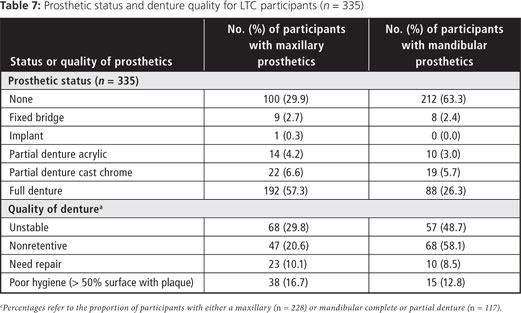
Forty-one percent of participants were edentulous (Table 6). More had maxillary full or partial dentures (68%) than mandibular dentures (35%). Of those completely edentulous, 92.6% wore their upper dentures all of the time (including those who took their denture out at night). More than a third (36.0%) did not have or never wore their lower denture. Mandibular dentures, when worn, were more likely to be unstable than maxillary dentures (Table 7).
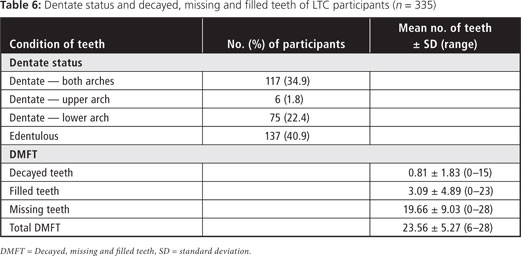
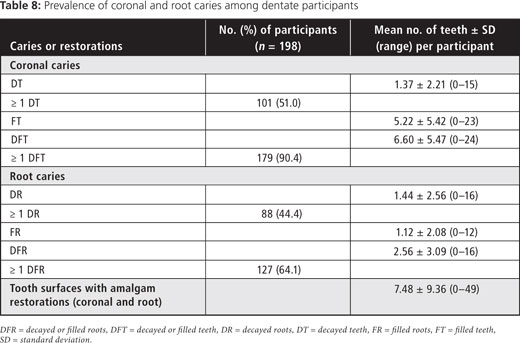
Among the dentate or partially dentate, there was a high caries rate (Table 8), on both coronal and root surfaces. The proportion with untreated root caries was similar to that with untreated coronal caries (44.4% versus 51.0%). Nearly two-thirds exhibited untreated or restored root caries on ≥ 1 teeth.
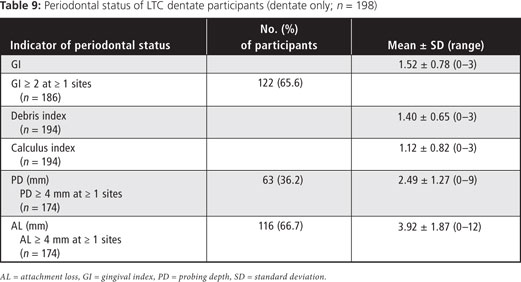
Two-thirds of participants had attachment loss of ≥ 4 mm, that is gingival recession, as reflected in the prevalence of root caries. About one-third of participants had ≥ 1 periodontal pockets of ≥ 4 mm depth (Table 9).
Predictors of Oral Disease
The most significant predictor of coronal decay was a high debris score, whereas perceiving a need for dental care was the most significant predictor of root caries (Table 9). Number of years of smoking (both current and former smokers) was a predictor for both root and coronal caries. Predictors of an increased DMFT score were increased age, years of smoking and brushing less than once a day (Table 10).
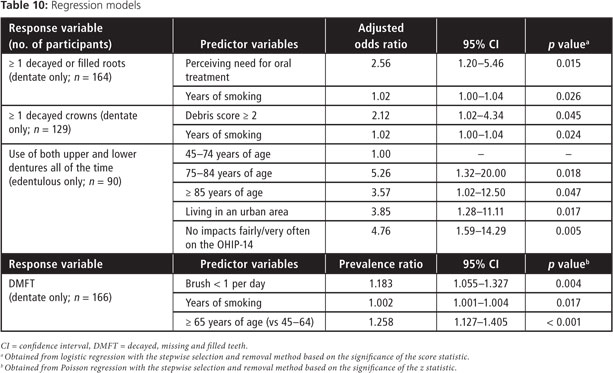
For the edentulous, the use of dentures (both upper and lower) all the time (except at night) was chosen as an indicator of oral health. Increased age, living in an urban area and infrequent impacts of oral conditions on oral health reported on the OHIP-14 (i.e., the prevalence of people reporting ≥ 1 item fairly often or very often, indicating a higher impact on oral health-related quality of life) were all predictors of regular denture use (Table 10).
Discussion
Challenges of Surveying in LTC
The main challenges of working in LTC settings were related to recruitment and space limitations. Recruitment of an adequate sample size was difficult because of the requirement that participants be able to provide informed consent and cancellations because of fatigue or illness. We dealt with this problem by overbooking appointments and extending the number of sampling days. Many facilities had limited space to accommodate the survey. The survey team used their portable dental chair and light in boardrooms, offices, activity rooms and hair dressing salons. The latter location worked well because there was a sink where the clinician could wash, and the chairs were adaptable for the clinical examination.
Implications of Results
The disease prevalence rates for this population of LTC residents fell within the ranges reported by other studies of institutionalized older people in industrialized countries. For example, 41% of participants in our study were edentulous compared with rates of 25%–64% in other studies5,19-22; 51% of our dentate participants had untreated coronal caries compared with 50%–68% reported in other studies5,21-22; and 44% of our participants had untreated root decay compared with reported rates of 46%–88% in other studies.5,22 Mean DMFT in this study (23.6) also fell within the range of 22.8–26.6 reported in other studies.5,22
Given the frailty of the population examined in our study, it is not surprising that a high proportion of the older participants experienced oral health problems. Self-care impairment is endemic in the nursing home population because of impaired visual acuity and decreased manual dexterity. LTC residents often rely on personal care-workers, who may be overloaded with daily work and may have little training in oral disease management23,24 for daily oral care. Further, personal care workers often view mouth care as more disagreeable than other nursing activities.23,24 Often LTC facilities do not enforce oral care policies.25 In addition few LTC facilities in Nova Scotia have access to professional oral care,26 which is reflected in the fact that two-thirds of the participants in our study had no regular dental care. Even if LTC residents are able to visit a dental care provider in the community, few have the financial means to do so.26 Recent changes to provincial legislation that allow dental hygienists to be self-regulated may alleviate some of the oral care burden. However in Nova Scotia, hygienists can provide limited restorative therapy only under the supervision of a dentist. Because caries is prevalent in this population, much of the oral disease will remain untreated.
Recent policy recommendations for improving the oral health of LTC residents encompass a wide range of workforce and system strategies. These include reforming the oral health care reimbursement system,3 educating oral health professionals to deal with the needs of frail and dependent older adults, developing standards for daily oral hygiene for LTC residents,3,27 educating institutional staff and using existing oral health professionals in new ways.27
Study Limitations
A lack of readily accessible data about the sociodemographic characteristics of LTC residents in Nova Scotia makes comparisons to the target population difficult. Because many residents were ineligible for our study because they were unable to give informed consent, we did not expect the sample from this survey to be representative of all LTC residents in Nova Scotia. Indeed, it is likely that the residents not represented (because of poor health or inability to give informed consent) have worse oral health status than those sampled because a loss of cognitive and functional capacity is predictive of need for oral treatment in LTC residents.28 Thus, the disease prevalence rates revealed in this study are likely conservative estimates of the true prevalence.
The use of an on-site recruiter (director of care or nursing, recreation coordinator or administrator) introduced the possibility of selection bias. This bias could go in either of 2 directions, namely, selecting residents believed to have the greatest oral health needs or selecting residents who were cooperative or physically active. We suspect the latter because recruiters frequently reported being challenged to find enough residents who were both physically able and capable of giving informed consent. Again, this bias would underestimate the true prevalence of oral disease.
Conclusions
A small but increasing fraction of the older adult population lives in residential continuing care settings, yet this population is most in need of oral care because of their limited mobility, multiple health issues and general loss of autonomy. The data from our study show what problems exist and to what extent they are present in this population—data essential to the improvement of health services.
THE AUTHORS
References
- Nova Scotia Department of Seniors. Seniors statistical profile 2009. Halifax: Communications Nova Scotia; 2009, 104 p. Available: www.gov.ns.ca/seniors/pub/2009_StatProfile.pdf (accessed 2012 Jan 17).
- Health Canada. Report on the findings of the oral health component of the Canadian Health Measures Survey 2007-2009. Ottawa: Publications Health Canada; 2010. 111 p. Available: www.fptdwg.ca/English/e-documents.html (accessed 2012 Jan 17).
- Canadian Dental Association. Report on seniors' oral health care. 2008. Available: www.jcda.ca/uploads/pdf/ccsa/Report-on-Seniors-Oral-Health-Care-2008-05-08.pdf (accessed 2012 Jan 17).
- Winn DM, Brunelle JA, Selwitz RH, Kaste LM, Oldakowski RJ, Kingman A, et al. Coronal and root caries in the dentition of adults in the United States, 1988-1991. J Dent Res. 1996;75(Spec No):642-51.
- Wyatt CC. Elderly Canadians residing in long-term care hospitals: part II. Dental caries status. J Can Dent Assoc. 2002;68(6):359-63.
- Thomson WM. Issues in the epidemiological investigation of dry mouth. Gerodontology. 2005;22(2):65-76.
- Gueiros LA, Soares MS, Leâo JC. Impact of ageing and drug consumption on oral health. Gerodontology. 2009;26(4):297-301. Epub 2009 Apr 8.
- Dolan TA, Atchison K, Huynh TN. Access to dental care among older adults in the United States. J Dent Educ. 2005;69(9):961-74.
- Quinonez C, Locker D, Sherret L, Grootendorst P, Azarpazhooh A, Figueiredo R. An environmental scan of publicly funded dental care in Canada. Community Dental Health Services Research Unit, Faculty of Dentistry, University of Toronto. Available: www.fptdwg.ca/assets/PDF/Environmental_Scan.pdf (accessed 2012 Jan 17).
- Nova Scotia Department of Seniors. Seniors statistical profile 2005. Halifax: Communications Nova Scotia; 2009, 78 p. Available: www.gov.ns.ca/seniors/publications.asp (accessed 2012 Jan 17)
- Albandar JM, Brunelle J, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70(1):13-29.
- duPlessis V, Beshiri R, Bollman RD, Clemenson H. Definitions of 'rural'. Ottawa: Statistics Canada; 2002. 37 p. Agriculture and Rural Working Paper Series No. 61, Catalogue no. 21-601-MIE.
- Statistics Canada. Canadian Health Measures Survey: Cycle 1 — 2007 to 2009 — Household questionnaire. Ottawa: Statistics Canada; 2006. 166 p. Available: www.statcan.gc.ca/imdb-bmdi/instrument/5071_Q2_V1-eng.htm#a1(accessed 2012 Jan 17).
- Slade G. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol.1997;25(4):284-90.
- Statistics Canada. Canadian Health Measures Survey Cycle 1 — 2007 to 2009 — Clinic questionnaire. Ottawa: Statistics Canada; 2006. 105 p. Available: www.statcan.gc.ca/imdb-bmdi/instrument/5071_Q1_V1-eng.htm (accessed 2012 Jan 17).
- Okeson J. Orofacial pain. Guidelines for assessment, diagnosis and management. Chicago: Quintessence Publishing Company; 1996.
- Vervoorn J, Duinkerke A, Luteijn F, Bouman T, van de Poel A. Reproducibility of an assessment scale of denture quality. Community Dent Oral Epidemiol. 1987;15(4):209-10.
- Statistics Canada. 2007. Nova Scotia (Code12) (table). 2006 Community Profiles. 2006 Census. Statistics Canada Catalogue no. 92-591-XWE. Ottawa. Released March 13, 2007. Available: http://www12.statcan.ca/census-recensement/2006/dp-pd/prof/92-591/index.cfm?Lang=E (accessed January 17, 2012).
- Kim HY, Jang MS, Chung CP, Paik DI, Park YD, Patton LL, et al. Chewing function impacts oral health-related quality of life among institutionalized and community-dwelling Korean elders. Community Dent Oral Epidemiol. 2009;37(5):468-76. Epub 2009 Jul 22.
- Tramini P, Montal S, Valcarcel J. Tooth loss and associated factors in long-term institutionalised elderly patients. Gerodontology. 2007;24(4):196-203.
- Shimazaki Y, SohI, Koga T, Miyazaki H, Takehara T. Relationship between dental care and oral health in institutionalized elderly people in Japan. J Oral Rehabil. 2004;31(9):837-42.
- Chalmers JM, Carter KD, Fuss JM, Spencer AJ, Hodge CP. Caries experience in existing and new nursing home residents in Adelaide, Australia. Gerondontology. 2002;19(1):30-40.
- Dharamsi S, Jivani K, Dean C, Wyatt C. Oral care for frail elders: knowledge attitudes and practices of long-term care staff. J Dent Educ. 2009;73(5):581-8.
- Jablonski RA, Munro CL, Grap MJ, Elswick RK. The role of biobehavioural, environmental, and social forces on oral health disparities in frail and functionally dependent nursing home elders. Biol Res Nurs. 2005;7(1):75-82.
- Pyle MA, Jasinevicius TR, Sawyer DR, Madsen J. Nursing home executive directors' perception of oral care in long-term care facilities. Spec Care Dent. 2005;25(1):111-7.
- McNally ME, Lyons R. The silent epidemic of oral disease: evaluating continuity of care and policies for the oral health care of seniors. Atlantic Health Promotion Research Centre; April 2004. Available: www.nsdental.org/media_uploads/pdf/58.pdf (accessed 2012 Jan 17).
- MacEntee MI, MacInnis B, McKeown L, Sarrapuchiello T. Dignity with a smile: oral healthcare for elders in residential care. A report for the Federal Dental Advisory Committee. 2008. Available: www.fptdwg.ca/assets/PDF/0901-Dignity%20with%20a%20Smile%20Final.pdf (accessed 2012 Jan 17).
- Nordernram G, Ljunggren G. Oral status, cognitive and functional capacity versus oral treatment need in nursing home residents: a comparison between assessments by dental and ward staff. Oral Dis. 2002;8(6):296-302.
