Abstract
In this clinical report, we describe the medical history, diagnosis and prosthodontic treatment of a 61-year-old man with a previous history of oral cancer. Loss of a full upper denture and severe erosion of his teeth prompted the patient to seek treatment at the dental clinic at the British Columbia Cancer Agency. Although he stated that he was being treated for a sleeping disorder, hospital records revealed multiple recent admissions for alcoholism and depression. The patient’s limited finances prevented complex restoration of worn lower dentition; thus, definitive treatment consisted of extraction of teeth with a poor prognosis, removal of a glandular odontogenic cyst and fabrication of a full maxillary prosthesis and a removable mandibular cast-metal overlay.
Many dentists rely on self-reported medical history acquired before treating a patient using a standard medical questionnaire. This is a quick, low-cost means to identify medical conditions and screen for disorders that might require consultation with a physician.1 However, self-administered medical questionnaires have been criticized for their inaccuracy; a patient may fail to report a condition as a result of forgetfulness, unwillingness to disclose information, misunderstanding of a disease or underestimating its significance.2,3 Imprecision may occur because of poor communication with the health care provider, particularly for diseases that are difficult to understand, fluctuate in course or lack clear diagnostic criteria.2,4 Mental disorders and alcoholism have been associated with underreporting of co-existing medical conditions.5
If the reliability of a patient’s self-reported medical history is questionable, the dentist should contact his or her physician or attempt to obtain all available medical records from clinics or hospitals before commencing treatment. The purpose of this clinical report is to describe the prosthodontic treatment and management of a patient who provided an elusive medical history.
Clinical Report
In September 2011, a 61-year-old man presented at the British Columbia Cancer Agency’s dental clinic in Vancouver, B.C., wanting a new complete maxillary denture as soon as possible, as he had lost his previous one.
In 1999 and 2009, he had been treated for oral cancer. The last available dental chart entry, made in May 2011, noted “an unstable maxillary complete denture with severely worn uneven occlusal surfaces and an occlusal plane slanting to the left probably due to parafunctional habits; but the patient has limited finances at this time and is unwilling to proceed with any dental treatments.”
The patient’s self-reported medical history included bilateral thrombosis in his lower extremities treated with vascular repairs, bronchitis, diverticulitis and oral squamous cell carcinoma (SCC) treated with radiation in 1999 and surgically resected in 2009 following a recurrence. He was taking trazodone (100 mg at bedtime) for insomnia. He had no primary care physician or dentist of record. According to the patient, his last hospital visit was in July 2011 to treat a “minor heart attack” and a “sleeping disorder.” He has smoked approximately 10 cigarettes a day for the past 40 years, but denied any recent alcohol consumption.
With the patient’s permission, hospital records were requested. They revealed a history of alcohol abuse that had resulted in admission for alcohol intoxication and delirium tremens in June and July 2011. He was being treated for depression in the psychiatric unit and had admitted to having suicidal thoughts. In addition, he was unemployed and had no home address.
On initial examination, the patient was alert and comfortable. Vital signs were within normal limits. Loss of muscle tone was apparent on the lower right side of the face and lip; this was associated with nerve damage related to resection of his recurrent SCC in the right lingual retromolar trigone. No palpable lymphadenopathy was apparent. Maximum oral opening was limited to 30 mm and elicited mild pain in the right inferior masseter muscle. Intraorally, the mucosa was intact and saliva was normal. The maxillary residual ridge appeared healthy but vestibular height was limited. There was no clinical evidence of dysplasia or recurrence of his SCC.
Oral hygiene was fair, although carious lesions were present on teeth 36, 37, 43, 44, 45 and 46. Mandibular teeth exhibited moderate attrition and erosion (Fig. 1). Significant loss of bone and attachment was noted around teeth 36, 37 and 46. Panoramic and periapical films revealed a radiolucency associated with a bony-impacted tooth 38, caries approaching the pulp in teeth 45 and 46 and furcation radiolucencies associated with teeth 36, 37 and 46 (Figs. 2 and 3).
 Figure 1: Pretreatment clinical photograph showing moderate attrition and erosion of mandibular teeth.
Figure 1: Pretreatment clinical photograph showing moderate attrition and erosion of mandibular teeth.
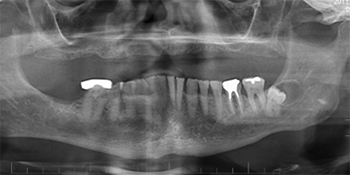 Figure 2: Pretreatment panoramic radiograph showing severe resorption of the maxilla, remaining mandibular teeth and radiolucency associated with tooth 38.
Figure 2: Pretreatment panoramic radiograph showing severe resorption of the maxilla, remaining mandibular teeth and radiolucency associated with tooth 38.
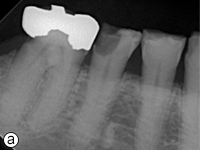
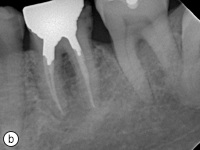
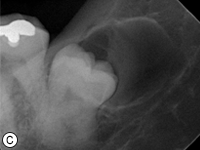
Figure 3: Periapical radiographs showing (a) caries lesions in teeth 46 and 45 (b) furcation radiolucencies in teeth 36 and 37 and (c) glandular odontogenic cyst associated with tooth 38
Taking into account cost of treatment and the patient’s medical and dental history, it was decided to avoid extensive rehabilitation (Table 1). The patient’s priority was construction of a new maxillary complete denture, and he accepted the option of an overlay removable partial denture that would restore the height of his mandibular teeth without crowns, help stabilize the occlusion, improve function and, possibly, increase the longevity of his prostheses. The treatment plan consisted of extraction of teeth with a poor prognosis (i.e., 36, 37, 45 and 46), extraction of tooth 38, biopsy of the associated radiolucency to rule out cancer recurrence, direct restoration of teeth 43 and 44 and fabrication of a maxillary complete denture and a mandibular cast-metal overlay removable partial denture.
The patient was referred to an oral surgeon for the extractions and biopsy, which was diagnosed as a glandular odontogenic cyst. Two weeks later, amalgam restorations of teeth 43 and 44 were carried out, and preliminary impressions were made and poured using type III dental stone (Microstone; Whip Mix Corp., Louisville, Ky.). Custom trays were fabricated using light polymerized resin (Triad; Dentsply Prosthetics, York, Pa.) and border molded with greenstick compound (impression compound; Kerr Corporation). A maxillary final impression was made with polysulfide impression material (Permlastic; Kerr Corporation) (Fig. 4) and poured using type III dental stone (Microstone). An occlusal rim was fabricated with acrylic (SR Ivolen; Ivoclar Vivadent) and pink wax (set-up wax, Patterson Dental, Saint Paul, Minn.). A fox plane was used to adjust the maxillary occlusal rim and records were completed using a facebow (Hanau facebow; Whip Mix Corp.) transfer to an articulator (Hanau H2XO; Whip Mix Corp.).
Table 1: Advantages and disadvantages of using overlay removable partial dentures in restoring vertical dimension
| Advantages | Disadvantages |
|---|---|
| Cost-effective | Possibility of caries if patient doesn’t maintain proper oral hygiene |
| Short treatment time | Potential maintenance issues associated with acrylic resin fracture and discoloration |
| Minimally invasive | Future difficulty in restoring teeth under the framework while maintaining the fit of the framework |
The mandibular study cast was surveyed, and parallel guiding planes were prepared on teeth 44 and 35. A final impression of the mandible was taken with light- and medium-bodied vinylpolysiloxane impression material (Aquasil Ultra; Dentsply Caulk, Milford, Del.), poured using type IV dental stone (Silky-Rock; Whip Mix Corp.) and the metal framework for an overlay denture was waxed and cast in chromium cobalt alloy. Acrylic (SR Ivolen) was added on the distal ends of the framework for an altered cast impression, which was taken 8 weeks after the extractions using light-bodied vinylpolysiloxane (Aquasil Ultra) and was poured in conjunction with the master cast in type III dental stone (Microstone) (Fig. 5). Wax-rims were fabricated for each distal extension and adjusted to be parallel to the maxillary occlusal rim. The occlusal vertical dimension was established using the combined methods of vertical dimension at rest, phonetics, aesthetics and function.6 Bite registration in centric relation was then taken with vinylpolysiloxane (Blue-Mousse; Parkell Inc., Edgewood, NY) and the mandibular master cast was mounted on the articulator. Maxillary anterior teeth (Ivoclar Vivodent Mold A22 in shade A3) were positioned according to anatomic landmarks and the patient’s feedback regarding aesthetics. Considering the patient’s grinding habit, 0° maxillary and mandibular posterior teeth were chosen and set on the residual ridge following a tooth-to-tooth bilateral balance scheme. The right side was set in cross-bite because of discrepancies in residual ridge size. The mandibular premolar and anterior teeth were waxed onto the framework of the removable partial denture with green wax (InStep Green Margin Wax, Whip Mix Corp.) (Fig. 6). Esthetics and phonetics were verified.
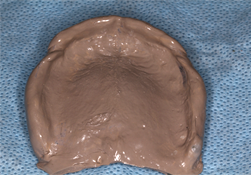 Figure 4: Final impression taken for the maxillary complete denture.
Figure 4: Final impression taken for the maxillary complete denture.
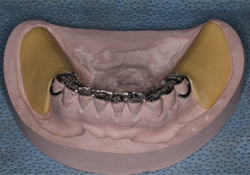 Figure 5: Cast-metal framework for the mandibular removable partial denture.
Figure 5: Cast-metal framework for the mandibular removable partial denture.
 Figure 6: Maxillary and mandibular occlusal rims with prosthetic teeth set-up with the wax-up of the mandibular premolar and anterior teeth in green wax on the cast metal framework, mounted on an articulator.
Figure 6: Maxillary and mandibular occlusal rims with prosthetic teeth set-up with the wax-up of the mandibular premolar and anterior teeth in green wax on the cast metal framework, mounted on an articulator.
Following esthetic approval by the patient, the dentures were prepared. The removable partial denture was constructed in two stages: first, pink acrylic resin was packed for the distal extensions, then shade VitaA3 acrylic was added for the anterior overlay. Both dentures were inserted into the patient’s mouth. The intaglio was verified and adjusted using pressure-indicating paste and occlusion was checked with articulating paper. The patient was given oral and denture hygiene instructions and a 6-month recall schedule with hygiene was recommended.
The patient returned twice for follow-up and adjustments. He was very satisfied with the fit and esthetics of the prostheses (Fig. 7). With his “new smile,” he felt motivated to return to work full time. He was able to eat more solid foods and felt that his bite had improved.


Figure 7: Patient with maxillary complete denture and mandibular removable partial denture in place: (a) view of prostheses and (b) esthetic appearance.
Conclusion
The patient described in this clinical report did not have a primary care physician and had attended various hospitals and walk-in clinics for treatment of alcoholism and depression. We speculate that he may have felt too embarrassed to disclose the details of his medical condition.
The mandibular cast-metal overlay removable partial denture was a cost-effective and efficient treatment for loss of occlusal vertical dimension, although its disadvantages include compromised esthetics and potential maintenance issues associated with acrylic resin fracture and discoloration (Fig 7).7 Poor oral hygiene also increases the risk of caries or periodontal disease.7 During treatment, regular weekly dental appointments were scheduled with the same clinician, except for the extractions which were carried out at a private practice nearby. This establishment of a patient–dentist connection may have contributed to the successful treatment outcome and acceptance of the removable prostheses. However, future follow-up visits are required to validate this.
THE AUTHORS
References
- Skinner KM, Miller DR, Lincoln E, Lee A, Kazis LE. Concordance between respondent self-reports and medical records for chronic conditions: experience from the Veterans Health Study. J Ambul Care Manage. 2005;28(2):102-10.
- Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145(8):762-9.
- Goldman N, Lin IF, Weinstein M, Lin YH. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol. 2003;56(2):148-54.
- Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al. Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology. Health Technol Assess. 2005;9(10):1-93, iii-iv.
- Meszaros ZS, Dimmock JA, Ploutz-Snyder R, Chauhan SV, Abdul-Malak Y, Middleton FA, et al. Accuracy of self-reported medical problems in patients with alcohol dependence and co-occurring schizophrenia or schizoaffective disorder. Schizophr Res. 2011;132(2-3):190-3.
- Turell AJ. Clinical Assessment of Vertical Dimension. J Prosthet Dent. 2006;96(2):79-83.
- Ganddini MR, Al-Mardini M, Graser GN, Almog D. Maxillary and mandibular overlay removable partial dentures for the restoration of worn teeth. J Prosthet Dent. 2004;91(3):210-4.


