ABSTRACT
The Canadian population is aging, and the oral health needs of this aging population have changed. The majority of older people are now dentate, which means that they continue to need the services of a dentist, specifically dentists who have been trained in geriatric oral health care. This paper reviews the history of geriatric training in Canada. Such training remains inadequate at both the predoctoral level and the postdoctoral or fellowship level. If geriatric or special needs dentistry were to be accepted as a specialty program, it might become more attractive as a career path for dentists.
Introduction
The world's population, including that of Canada, is aging.1 Between 1956 and 2001, the proportion of the Canadian population 65 years of age and older rose from 7.7% to 13%2 and by 2031, this value is expected to reach more than 20%.2 The 2006 census reported that in the past 5 years, the number of people over age 64 had increased by 11.5%,3 and by 2020, it is predicted that seniors will outnumber children in every province, with a median national age of 44 years.3 Furthermore, persons aged 80 years and older represent the fastest-growing age group in this country.4
This aging cohort differs from elderly persons of the past: seniors today are better educated, are more politically aware and accept social services more readily than their past counterparts. As a group, they are more economically secure and may be healthier, but more importantly for the dental profession, these individuals have retained many of their natural teeth.5 These older adults have a higher risk for new coronal and root caries and recurrent caries than younger cohorts, as removing plaque becomes more difficult and complex due to poor vision, reduction in hand–eye coordination and age-related recession.6 Hypofunction of the salivary glands and xerostomia affect about 30% of this population, creating potential difficulties with mastication, gustation and swallowing; these problems also pose a higher risk of oral mucosal problems and may contribute to inappropriate nutritional selection.7 Members of this older cohort who remain functionally independent can be expected to seek dental care that is similar to that provided to younger dentate persons.8 Although many older people have complex restorative problems, such as bone loss due to periodontal disease, caries and unresolved periapical pathology, they will be less willing to accept the simple solutions of the past, such as extraction of their remaining natural teeth and construction of complete dentures.9
History of Geriatric Dental Education
In the 1970s, anticipation of the aging of the baby boomers resulted in recognition of the coming need for dental health practitioners with knowledge about geriatric dentistry. In a review published in the year 2000, Leake10 reported that the Canadian Dental Association's Council on Public Health had identified problems in caring for elderly patients as early as 1967. At the time, geriatric dentistry had only a token presence in the curricula of Canadian dental schools, usually as part of another dental discipline's lecture or seminar series. In 1992, Vincent and colleagues11 stated that Canadian dental schools had no specific courses in geriatric dentistry. The most recent published study about geriatric dentistry teaching in Canadian dental schools is now more than 10 years old.12 At the time of publication of that study, in 1998, only 3 (33%) of the 9 Canadian dental schools had a required didactic course in geriatric dentistry, whereas 46 (88%) of the 52 US schools had such courses (Table 1). In terms of clinical teaching, 4 (44%) of the Canadian schools had a special rotation in geriatric dentistry, which was comparable to the 28 (54%) US dental schools with such a rotation (Table 2). No data are available to illustrate the changes that have occurred in Canadian dental schools since 1998, but based on word-of-mouth anecdotal evidence, most Canadian dental school curricula now have a required course in geriatric dentistry. In my opinion, that one didactic course without supporting clinical experiences is insufficient at the predoctoral level. I also believe there is a need to develop postdoctoral and fellowship programs in geriatric dentistry, to train the teachers and consultants of the future.
Table 1 Didactic teaching of geriatric dentistry in Canada and the United States, 1998a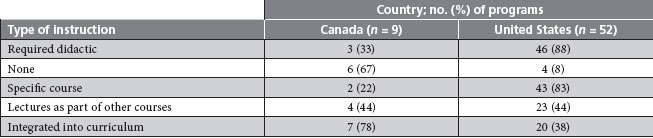
aSource of data: Saunders RH et al.12
Table 2 Sites of clinical teaching of geriatric dentistry in Canada and the United States, 1998a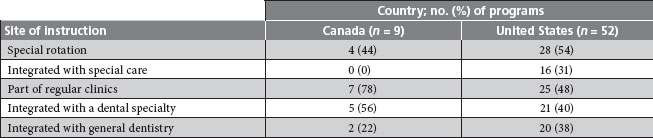
aAdapted with permission from Saunders RH et al.12
In a 2002 survey of graduating classes from US dental schools,13 20% of the 3646 respondents stated that they were "less than or not well prepared" to provide care for older adults. In the same study, nearly 25% stated that insufficient time had been allocated for geriatric dental care in their dental school curricula. These same students ranked geriatric dentistry fourth in a list of subjects that had been taught inadequately during their dental training.
Workforce Issues and Postgraduate Training
The 2000 US Surgeon General's report on oral health14 stated that older adults suffered from a "silent epidemic of profound and consequential dental problems." Teachers and clinicians will therefore be required to care for this population's oral health needs. A US Department of Health and Human Services report to Congress15 projected a need for at least 6000 dental practitioners with substantial training in geriatric dentistry by the year 2020. The report's authors also foresaw a need for an additional 2000 dentists with no formal training but with clinical experience in treating this population. If the conclusions of this report are extrapolated to Canada, which has about 10% of the population of the United States, this country will need at least 600 fully trained geriatric dentists and 200 minimally trained dentists to care for its aging population in 2020.
Since the 1980s, national funding has been available in the United States to develop geriatric dental curricula and to train clinicians in geriatric dentistry (Table 3). The total number of dentists that have been trained to date through these programs does not exceed 200, which falls far short of the projected requirement identified for 2020. As such, there is a great need to identify suitable candidates, to train them and then to find jobs for them in academia, as well as in the public and private sectors. No such formal training programs have been available in Canada, but the dental schools at the University of British Columbia and Laval University have master's programs in geriatric dentistry. Positions in these programs have sometimes gone unfilled, so it is difficult to estimate the number of trained geriatric dental clinicians in Canada.
Table 3 Postgraduate geriatric education in the United States
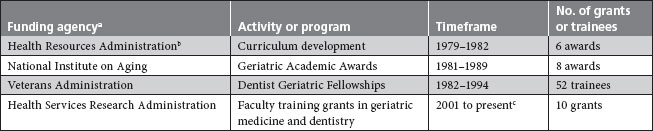
aNational funding sources for development of curricula and clinical training programs became available starting in the 1980s. As of 2009, a total of between 150 and 200 people had been trained.
bHealth Resources Administration and Health Services Administration merged in 1982 to create Health Resources and Services Administration.
cThe Health Services Research Administration currently administers ten 2-year programs.
Several US initiatives launched in the 1990s resulted in a white paper on oral health,16 which made specific recommendations, identified expected outcomes and set up a timetable to achieve these goals. Some of these recommendations are listed in Box 1.
Several of these recommendations have already been implemented by US dental schools. However, several problems remain unresolved in the United States:
Box 1 Recommendations for geriatric dental education16
Predoctoral dental and allied dental education and training programs:
- Develop, implement, and evaluate geriatric dentistry clinical competencies and education standards
- Require dental school accreditation standards for geriatrics education
- Establish core competencies in national dental and dental hygiene boards and regional/state licensure board examinations
- Educate all health professional students in the principles of interdisciplinary team management and include the oral needs of older patients
- Employ continuous quality improvement in dental education and in the dental care of older patients
Postdoctoral education and training in geriatric dentistry:
- Increase the number of postdoctoral general dentistry training programs
- Increase the number of postdoctoral academic training opportunities for dental faculty
- Offer advanced geriatric training in postdoctoral general dentistry training programs
- Increase the numbers and types of alternative pathways to geriatric education for dental professionals, to encourage lifelong learning
- There is no established career structure for people graduating from any of the US programs in geriatric dentistry, unless they also complete a master's degree in public health, dental public health or a similar area.
- Current salaries in the United States for academics and hospital dentists are not competitive with salaries in the private sector; at the same time, hospital administrators are questioning the credentials of dentists now working in hospitals, as these professionals do not have specialty status.
- Students have a large debt load upon graduation, which makes academic and hospital dentistry careers unattractive; as such, dental schools are unable to attract young or middle-level faculty even though they are needed to replace the current faculty, who are aging.
- Reimbursement for the care of indigent populations, including older adults, varies by state; at best, such reimbursement covers the dentist's overhead.
Changes in geriatric dentistry are now occurring worldwide:
- Brazil was the first country to recognize the specialty of geriatric dentistry in 2001.17
- New Zealand has a 3-year graduate program in special needs dentistry that includes geriatrics. This program is under the auspices of the Royal Australasian College of Dental Surgeons, which grants specialty status after an examination.
- In Australia, the states of Victoria and South Australia have programs that are similar to that offered in New Zealand.
- In the United Kingdom, consultancies in special needs dentistry have been established.
- In the United States, the Special Care Dentistry Association (SCDA) has developed a diplomate program in geriatric and special needs dentistry. The first diplomate examinations will be held during the association's annual meeting in Chicago in 2010. Once the program is well established, the SCDA will apply to the American Dental Association for specialty status.
Accreditation criteria for US dental schools now include requirements for instruction in geriatric dentistry. In 2006, the Commission on Dental Accreditation added the following statement for a new standard on patients with special needs, including geriatric patients: "Graduates must be competent in assessing the treatment needs of patients with special needs … patients whose medical, physical, psychological, or social situations may make it necessary to modify normal dental routines in order to provide dental treatment for that individual. These individuals include, but are not limited to, people with developmental disabilities, complex medical problems, and significant physical limitations."18 No such accreditation requirement currently exists in Canada.
Barriers
The barriers to teaching geriatric dentistry have been known for some time. These were highlighted by Moshman and colleagues19 in 1985 and were further defined by Ettinger and colleagues20 in 2004. The 3 main barriers relate to curriculum time, funding and training of faculty:
- The dental curriculum is already overcrowded, and there is competition among the disciplines for instructional time; nobody wants to sacrifice time currently devoted to their respective specialties to allow time for geriatric training.
- There is a lack of faculty positions, and no discipline wishes to give up a full-time equivalent position to allow hiring of a specialist in geriatric dentistry.
- There are a limited number of training programs and trained personnel worldwide, and it is hard to recruit qualified faculty to existing positions.
Conclusion
There is a geriatric imperative in Canada. Several regional studies have shown that the people in the aging Canadian population are maintaining their natural teeth and will continue to need oral health care. The Canadian Dental Association and Canadian dental schools must determine the number of practitioners that will be needed and the expertise that these practitioners will require. In addition, ways must be found to attract dentists to become teachers and consultants in geriatric and special needs dentistry. One solution might be to provide a pathway to specialization, to give dentists a more defined career structure in academia, in public service and in private practice.
THE AUTHOR
References
- Kinsell K, Wan W. US Census Bureau, International Population Reports, P95/09-1, An Aging World: 2008, US Government Printing Office, Washington, D.C., 2009.
- Statistics Canada. Canadian Social Trends. Census snapshot of Canada – Population (age and sex). December 11, 2007. Available: www.statcan.gc.ca/pub/11-008-x/2007006/article/10379-eng.pdf (accessed 2010 Jan 14).
- Canada's population is aging at an alarming rate: 2006 census. LefeSiteNews website. Published July 26, 2007. Available: www.lifesitenews.com/ldn/2007/jul/07072603.html (accessed 2010 Jan 14).
- Population Division, United Nations. World population ageing: 1950-2050. New York: United Nations, 2001. Available: www.un.org/esa/population/publications/worldageing19502050/ (accessed 2010 Jan 14).
- Ettinger RL, Beck JD. The new elderly: what can the dental profession expect? Spec Care Dentist. 1982;2(2):62-9.
- Chalmers JM, Carter KD, Spencer AJ. Caries experience and increments in community-living older adults with and without dementia. Gerodontology.2002;19(2):80-94.
- Thomson WM, Chalmers JM, Spencer AJ, Slade GD. Medication and dry mouth: findings from a cohort study of older people. J Public Health Dent. 2000;60(1):12-20.
- Brothwell DJ, Jay M, Schonwetter DJ. Dental service utilization by independently dwelling older adults in Manitoba, Canada. J Can Dent Assoc. 2008;74(2):161. Available: www.cda-adc.ca/jcda/vol-74/issue-2/161.html.
- Ettinger RL, Mulligan R. The future of dental care for the elderly population. J Calif Dent Assoc. 1999;27(9):687-92.
- Leake JL. The history of dental programs for older adults. J Can Dent Assoc. 2000;66(6):316-9.
- Vincent JR, Massicotte P, Barolet RY. The teaching of geriatric dentistry in Canada. J Can Dent Assoc. 1992;58(9):731-5.
- Saunders RH, Yellowitz JA, Dolan TA, Smith BJ. Trends in predoctoral education in geriatric dentistry. J Dent Edu. 1998;62(4):314-8.
- Weaver RG, Haden NK, Valachovic RW; American Dental Education Association. Annual ADEA survey of dental school seniors: 2002 graduating class. J Dent Edu. 2002;66(12):1388-404.
- US Department of Health and Human Services. Oral health in America: report of the Surgeon General. Rockville, Maryland: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2000. Available: www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/ (accessed 2010 Jan 14).
- National Institute on Aging. Personnel for health needs of the elderly through year 2020. Washington, DC: NIH Pub. No. 87-2950, 1987.
- Dolan TA, Berkey DB, Mulligan R, Saunders MJ. The state of the art of geriatric dental education and training. In: Klein SM (editor). A national agenda for geriatric education: white papers. New York: Springer Publishing Co.; 1995. p. 125-53.
- Hebling E, Mugayar L, Vendramini Dias P. Geriatric dentistry: a new specialty in Brazil. Gerodontology. 2007;24(3):177-80.
- Commission on Dental Accreditation. Accreditation standards for dental education programs. Standard 2-26. Published January 25, 2007. Modified February 1, 2008. Available: www.ada.org/prof/ed/accred/standards/predoc.pdf (accessed 2010 Jan 14).
- Moshman J, Warren GB, Blandford DH, Aumack L. Geriatric dentistry in the predoctoral curriculum. J Dent Educ. 1985;49(10):689-95.
- Ettinger RL, Chalmers J, Frenkel H. Dentistry for persons with special needs: how should it be recognized? J Dent Educ. 2004;68(8):803-6.
