ABSTRACT
The restoration of teeth with extensive structural damage is an important clinical procedure in dental practice. However, despite the availability of a variety of materials, techniques and studies in the scientific literature, the criteria for selection of such teeth for restoration need clarification. The approach to severely compromised teeth should be based on consistent scientific evidence to reduce dental error and improve the prognosis. If restoration is indicated, it must conserve and protect the remaining tooth structure. In this article, we develop and suggest clinical criteria and guidelines that clinicians may use to identify and classify extensively damaged teeth to help in the diagnosis, treatment plan and prognosis.
Introduction
A tooth with extensive damage is one that has lost substantial structure as a result of caries, previous restoration failures, fractures or even procedures related to endodontic treatment. The restoration of such teeth with endodontic treatment is an important clinical procedure in dental practice; however, various studies have taken different perspectives on this issue.1,2 The loss of dental tissue and the weakening of the remaining structure present a challenge in terms of prosthetic rehabilitation. Although the current success rate of dental implants is high,3 the clinician must be able to assess the probability of restoring severely damaged teeth successfully.4-10 The dimensions of the remaining tooth tissues as well as several biological and occlusal factors must be properly assessed to establish the correct treatment plan.
The aim of this article is to present clinical guidelines to help the clinician easily diagnose and establish a treatment plan for the rehabilitation of severely damaged teeth.
Assessing the Probability of Successful Restoration
Remaining Tooth Tissues
The extent of the remaining tooth structure is among the most important and critical factors in determining the prognosis for restoration of a damaged tooth. Evidence indicates that the dimensions of the crown dentin are important.4 Some studies11,12 agree that a dentin thickness < 1 mm increases the risk of failure. This minimum thickness is more often achieved in buccal or palatal/lingual than interproximal areas after endodontic treatment and tooth preparation.4,13-15 The ferrule effect—the need for a 360º collar 2 mm in height (1.5 mm minimum)—was described by Sorensen and Engelman11 in 1990. Smaller dimensions are associated with a greater risk of failure.4,6,9,16-22
A post should be used only when there is insufficient tooth substance remaining to support core material or the final restoration. The height of the post should always be the same or greater than that of the future crown, and its width should be established by the width of the canal after root canal treatment. Increasing post diameter in an effort to increase retention is not recommended, as this creates unnecessary weakening of the remaining tooth structure.1,9,23-25
Biologic Considerations
Caries, previous restorations and fractures can affect the biologic width of the remaining structure and lead to accumulation of bacteria, inflammation, increased probing depth, gingival recession or a combination of these problems. When sulci are normal (2–3 mm) and healthy and bands of attached gingiva are adequate, margins can be placed up to 0.5 mm inside the sulcus. When tooth structure is insufficient to allow adequate soft tissue attachment, other procedures (such as surgical crown lengthening or orthodontic extrusion) may be necessary to achieve optimal results.26-34
In preparing a root canal for a post, the main barrier against reinfection of the periapical region is the endodontic obturation material. The length of the remaining apical seal after post preparation can influence the long-term success of the restoration.4,5,10,35-38 There is some evidence for leaving 3–5 mm of undisturbed apical endodontic obturation material after post preparation. Only some teeth have a 1-mm thick layer of dentin 5 mm from the apex. At distances less than 3 mm from the apex, there is unlikely to be 1 mm of sound dentin surrounding the apical end of the post.4,10,39
Occlusal Factors
Occlusal load is also an important consideration in estimating the chances of successful restoration of a damaged tooth. In a retrospective study, Sorensen and Martinoff40 found that, although the success rate for single-unit crowns was 94.8%, it was 89.2% for fixed partial denture abutments and only 77.4% for removable partial denture abutments. Nyman and Lindhe41 found that fractures in abutment teeth occurred more frequently in root-treated teeth. Hatzikyriakos and colleagues42 reported a failure rate for endodontically treated teeth used as abutments for fixed and removable partial dentures that was more than twice that for such teeth not used as abutments.
Some conclusions can be drawn from these studies. Extensively damaged teeth cannot be considered reliable as abutments for fixed or removable dentures (especially long-span fixed bridges and distal extensions of removable dentures) or cantilevers or for patients with severe bruxism and clenching habits.4,8,9,11,41,42
Clinical Protocol for Diagnosing Extensively Damaged Teeth
For a severely damaged tooth, some elements of a treatment plan are mandatory:
- Removal of all caries and old restorations to achieve access to the remaining tooth structure.
- Elimination of all periodontal infection and control of plaque.
- Predetermination of the value of the tooth, e.g., is it important for occlusion or esthetics?
The following criteria should then be assessed in this sequence: ferrule effect, relation between root and crown length, endodontic condition.
Criterion 1 – Ferrule Effect
The ferrule effect is determined from vertical and horizontal intraoral measurements. The vertical measurement is from the top of the gingival margin to the top of the remaining tooth wall at 4 points: mesial, distal, buccal and lingual or palatine. This can be easily assessed using a periodontal probe with a stop and an endodontic ruler. Values are positive if the top of the remaining tooth is above the gingival margin (Fig. 1) or negative if it is below (Fig 2).
The horizontal measurement is the thickness of the remaining tooth walls at the level of the future crown margin at 4 points: mesial, distal, buccal and lingual or palatine (Fig. 3). This can be easily measured with calipers, which are commonly used to measure framework thickness of fixed prosthodontics (Fig. 4). If space does not permit the use of calipers, a periodontal probe (with a stop) can be used instead (Fig. 5).
 Figure 1: Measurement of the remaining buccal wall of tooth 15 with a periodontal probe and stop. The value is positive as the top of the remaining tooth is above the gingival margin.
Figure 1: Measurement of the remaining buccal wall of tooth 15 with a periodontal probe and stop. The value is positive as the top of the remaining tooth is above the gingival margin.
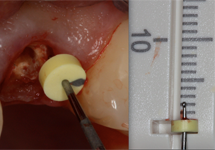 Figure 2: Measurement of the remaining buccal wall of tooth 22 with a periodontal probe and stop. The value is negative as the tooth wall is below the gingival margin.
Figure 2: Measurement of the remaining buccal wall of tooth 22 with a periodontal probe and stop. The value is negative as the tooth wall is below the gingival margin.
 Figure 3: Location of horizontal intraoral measurements.
Figure 3: Location of horizontal intraoral measurements.
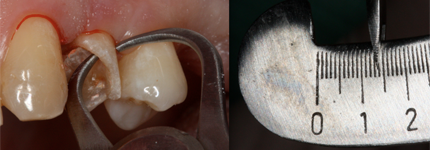 Figure 4: Measurement of the remaining buccal wall of a damaged tooth with calipers (1.4 mm).
Figure 4: Measurement of the remaining buccal wall of a damaged tooth with calipers (1.4 mm).
 Figure 5: Measurement of the remaining distal wall of a damaged tooth using a periodontal probe.
Figure 5: Measurement of the remaining distal wall of a damaged tooth using a periodontal probe.
Criterion 2 – Relation of Crown to Root Length
This factor is important in predicting the retention of the future restoration. As noted above, to promote retention of the crown, a post should be at least the same length as the future crown. Future crown length may be measured from the top of the supposed tooth to the hypothetical margin, intraorally or using a model (Fig. 6).
Root length may be measured radiographically (Fig. 7).
If needed, on a buccal (Fig. 8), palatine or lingual face, it is possible to measure the distance of the reference level to the top of the remaining tooth and transfer this measure to the radiograph (see d′ on Fig. 8). Then measure the root length from this level to the apex on the radiograph (see r′ on Fig. 8). Using the ratio of d to d′, calculate the real dimension of the root, r, from r′.
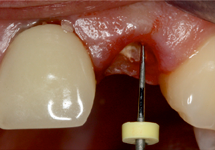 Figure 6: Measurement of an extensively damaged tooth 22 from the supposed top of the tooth to the hypothetical margin with a periodontal probe.
Figure 6: Measurement of an extensively damaged tooth 22 from the supposed top of the tooth to the hypothetical margin with a periodontal probe.
 Figure 7: Radiograph showing crown and root measurements.
Figure 7: Radiograph showing crown and root measurements.
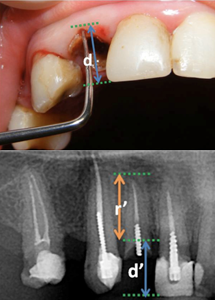 Figure 8: Determination of root length at the buccal face of tooth 12.
Figure 8: Determination of root length at the buccal face of tooth 12.
Criterion 3 – Endodontic Condition
The remaining tooth should be evaluated related to the extent of endodontic treatment required: can treatment be performed without predictable complications, are complications likely and, thus, treatment outcome is uncertain or are complications irreversible and cannot be resolved with endodontic treatment.
Classification of Teeth with Extensive Endodontic Damage
Class I
- Ferrule effect: Height of remaining tooth ≥ 2 mm at 4 locations (mesial, distal, buccal, palatine or lingual) and thickness of remaining tooth walls ≥ 2.2 mm for an esthetic restoration or ≥ 1.6 mm for non-esthetic restorations
- Remaining root length: At least as long as the future crown height plus 5 mm for the apical seal
- Endodontic condition: Endodontic treatment may be performed without predictable complications
- Prognosis: Good
Class II
- Ferrule effect: Height of remaining tooth 0.5–2 mm or width of remaining tooth walls 1.6–2.2 mm with visible margins or 1.2–1.6 mm with non-visible margins
- Remaining root length: Less than crown height plus 5 mm but equal or greater than crown height plus 3 mm
- Endodontic condition: Without predictable complications or with uncertain results
- Prognosis: Moderate
Note: A tooth in this class should not be used as an abutment. A new evaluation should be performed after endodontic treatment in cases where pretreatment prognosis is uncertain.
Class III
- Ferrule effect: Height of remaining tooth < 0.5 mm or width of remaining tooth wall < 1.2 mm at future margin level
- Remaining root length: Less than crown height plus 3 mm
- Endodontic condition: With irreversible complications
- Prognosis: Poor
Note: A tooth in this class is not a candidate for treatment; it should be extracted and replaced by a prosthesis.
The clinical record form below may be used to evaluate severely damaged teeth using these criteria. Each parameter is evaluated and individually classified as I, II or III. Final classification is the highest class for any parameter, i.e., a tooth rated I, II, I for the 3 parameters, is Class II.
Clinical record form for scoring teeth with extensive damage
| Class I, prognosis good |
Class II, prognosis moderate |
Class III, prognosis poor |
||||
| Ferrule effect | Height ≥ 2mm Width ≥ 2.2 mm (esthetic) ≥1.6 (non-esthetic) |
Height ≥ 0,5–2 mm Width 1.6–2.2 mm (visible margins) 1.2–1.6mm (non-visible margins) |
Height < 0.5mm Width < 1.2 mm |
|||
| Root length | ≥ crown height + 5 mm | < crown height + 5 mm ≥ crown height + 3 mm |
< crown length + 3 mm | |||
| Endodontic condition | Without predictable complications | Without predictable complications or uncertain treatment results | With irreversible complications | |||
Final classification _________________________
Additional Clinical Considerations
- Pre-prosthetic treatment may affect the initial classification.
- Concern about special stress patterns (bruxism, abutments for a removable partial denture, cantilevers, extensive bridges or secondary abutments) raises the class level from I to II or from II to III.
- Class level also increases by 1 if there are esthetic concerns.
- In cases where there is no antagonist, no occlusal issues, the antagonist is a removable denture or there is clinical evidence of small to no loads over the remaining tooth, the class level decreases by 1.
- For patients with poor oral hygiene, uncontrolled periodontal disease or caries, an extensively damaged tooth should be considered Class III.
Conclusion
Clinical guidelines help the dentist arrive at the correct diagnosis and treatment plan, avoid errors, increase the predictability of dental treatment and increase the quality of service. Although the literature describes the rehabilitation of teeth with extensive endodontic damage, no clinical guidelines have been published. Our goal in this article is to provide the clinician with such guidelines for selection of extensively damaged teeth for rehabilitation.
THE AUTHORS
References
- Cheung W. A review of the management of endodontically treated teeth. Post, core and the final restoration. J Am Dent Assoc. 2005;136(5):611-9.
- Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30(5):289-301.
- Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang H. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91.
- McLean A. Criteria for the predictably restorable endodontically treated tooth. J Can Dent Assoc. 1998;64(9):652-6.
- Whitworth JM, Walls AW, Wassell RW. Crowns and extra-coronal restorations: endodontic considerations: the pulp, the root-treated tooth and the crown. Br Dent J. 2002;192(6):315-20, 323-7.
- Goodacre CJ. Five factors to be considered when restoring endodontically treated teeth. Pract Proced Aesthet Dent. 2004;16(6):457-62.
- Morgano SM, Brackett SE. Foundation restorations in fixed prosthodontics: current knowledge and future needs. J Prosthet Dent. 1999;82(6):643-57.
- McLean A. Predictably restoring endodontically treated teeth. J Can Dent Assoc. 1998;64(11):782-7.
- Morgano SM, Rodrigues AH, Sabrosa CE. Restoration of endodontically treated teeth. Dent Clin North Am. 2004;48(2):vi,397-416.
- Goodacre CJ, Spolnik KJ. The prosthodontic management of endodontically treated teeth: a literature review. Part II. Maintaining the apical seal. J Prosthodont. 1995;4(1):51-3.
- Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63(5):529-36.
- Tjan AH, Whang SB. Resistance to root fracture of dowel channels with various thicknesses of buccal dentin walls. J Prosthet Dent. 1985;53(4):496-500.
- Shillingburg HT. Fundamentals of fixed prosthodontics. Quintessence Pub.Co.; 1997.
- Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 2008;39(2):117-29.
- Arunpraditkul S, Saengsanon S, Pakviwat W. Fracture resistance of endodontically treated teeth: three walls versus four walls of remaining coronal tooth structure. J Prosthodont. 2009;18(1):49-53.
- al-Hazaimeh N, Gutteridge DL. An in vitro study into the effect of the ferrule preparation on the fracture resistance of crowned teeth incorporating prefabricated post and composite core restorations. Int Endod J. 2001;34(1):40-6.
- Pereira JR, de Ornelas F, Conti PC, do Valle AL. Effect of a crown ferrule on the fracture resistance of endodontically treated teeth restored with prefabricated posts. J Prosthet Dent. 2006;95(1):50-4.
- Dorriz H, Alikhasi M, Mirfazaelian A, Hooshmand T. Effect of ferrule and bonding on the compressive fracture resistance of post and core restorations. J Contemp Dent Pract. 2009;10(1):1-8.
- Kutesa-Mutebi A, Osman YI. Effect of the ferrule on fracture resistance of teeth restored with prefabricated posts and composite cores. Afr Health Sci. 2004;4(2):131-5.
- Dikbas I, Tanalp J, Ozel E, Koksal T, Ersoy M. Evaluation of the effect of different ferrule designs on the fracture resistance of endodontically treated maxillary central incisors incorporating fiber posts, composite cores and crown restorations. J Contemp Dent Pract. 2007;8(7):62-9.
- Sendhilnathan D, Nayar S. The effect of post-core and ferrule on the fracture resistance of endodontically treated maxillary central incisors. Indian J Dent Res. 2008;19(1):17-21.
- Stankiewicz N, Wilson P. The ferrule effect. Dent Update. 2008;35(4):222-4, 227-8.
- Standlee JP, Caputo AA, Hanson EC. Retention of endodontic dowels: effects of cement, dowel length, diameter, and design. J Prosthet Dent. 1978;39(4):400-5.
- Kurer HG, Combe EC, Grant AA. Factors influencing the retention of dowels. J Prosthet Dent. 1977;38(5):515-25.
- Peroz I, Blankenstein F, Lange KP, Naumann M. Restoring endodontically treated teeth with posts and cores — a review. Quintessence Int. 2005;36(9):737-46.
- Padbury A Jr, Eber R, Wang HL. Interactions between the gingiva and the margin of restorations. J Clin Periodontol. 2003;30(5):379-85.
- Addy LD, Durning P, Thomas MB, McLaughlin WS. Orthodontic extrusion: an interdisciplinary approach to patient management. Dent Update. 2009;36(4):212-4, 217-8.
- Bach N, Baylard JF, Voyer R. Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc. 2004;70(11):775-80.
- Goldberg PV, Higginbottom FL, Wilson TG. Periodontal considerations in restorative and implant therapy. Periodontol 2000. 2001;25:100-9.
- Lovdahl PE. Periodontal management and root extrusion of traumatized teeth. Dent Clin North Am. 1995;39(1):169-79.
- Fugazzotto PA, Parma-Benfenati S. Preprosthetic periodontal considerations. Crown length and biologic width. Quintessence Int Dent Dig. 1984;15(12):1247-56.
- Magne P, Magne M, Belser U. The esthetic width in fixed prosthodontics. J Prosthodont. 1999;8(2):106-18.
- Kois JC. The restorative-periodontal interface: biological parameters. Periodontol 2000. 1996;11:29-38.
- Sterr N, Becker A. Forced eruption: biological and clinical considerations. J Oral Rehabil. 1980;7(5):395-402.
- Mattison GD, Delivanis PD, Thacker RWJr, Hassell KJ. Effect of post preparation on the apical seal. J Prosthet Dent. 1984;51(6):785-9.
- Grecca FS, Rosa AR, Gomes MS, Parolo CF, Bemfica JR, Frasca LC, et al. Effect of timing and method of post space preparation on sealing ability of remaining root filling material: in vitro microbiological study. J Can Dent Assoc. 2009;75(8):583.
- Haddix JE, Mattison GD, Shulman CA, Pink FE. Post preparation techniques and their effect on the apical seal. J Prosthet Dent. 1990;64(5):515-9.
- DeCleen MJ. The relationship between the root canal filling and post space preparation. Int Endod J. 1993;26(1):53-8.
- Peroz I, Blankenstein F, Lange KP, Naumann M. Restoring endodontically treated teeth with posts and cores — a review. Quintessence Int. 2005;36(9):737-46.
- Sorensen JA, Martinoff JT. Endodontically treated teeth as abutments. J Prosthet Dent. 1985;53(5):631-6.
- Nyman S, Lindhe J. Prosthetic rehabilitation of patients with advanced periodontal disease. J Clin Periodontol. 1976;3(3):135-47.
- Hatzikyriakos AH, Reisis GI, Tsingos N. A 3-year postoperative clinical evaluation of posts and cores beneath existing crowns. J Prosthet Dent. 1992;67(4):454-8.
