Abstract
We describe a case of complex trauma to the early mixed dentition in which tooth avulsion, intrusion, extrusion and lateral luxation were managed effectively using a fixed, non-rigid orthodontic splint after treatment with a traditional wire-composite splint had failed. The use of orthodontic brackets and flexible wires provided several advantages, such as the ability to splint severely malpositioned teeth; easy assessment without removing the splint; slow, gentle repositioning of traumatized teeth; and gradual reestablishment of the arch form allowing for ease of future prosthodontic rehabilitation. Therefore, orthodontic appliances should be considered as a viable option for managing complex dental trauma.
Dental trauma is common in the pediatric population, affecting approximately 1 in 3 children.1 Trauma to the mixed dentition can be complicated because of the varying stages of tooth eruption and root development.
Luxation injuries to the dentition are classified according to resulting tooth mobility and displacement.2 These injuries include concussion, subluxation, lateral luxation, extrusion, intrusion and avulsion. Potential complications include pulp necrosis, pulp canal obliteration, internal and external root resorption, cessation of root development, ankylosis and loss of marginal bone.2 The goal of management is to mitigate these complications and prevent tooth loss.
Splinting is the principle method for treating dental trauma, as splinting stabilizes the traumatized teeth, maintaining them within the periodontium, precluding further trauma and facilitating periodontal healing.3,4 Splinting is indicated when a tooth is displaced, avulsed or excessively mobile or for the comfort of the patient.
Ideally, the splinting procedure should be simple, fast and atraumatic. The splint should provide adequate stabilization and fixation; be esthetic, hygienic, passive and non-irritating; not interfere with occlusion; and allow for endodontic access, physiological mobility and easy assessment of teeth on follow-up visits.3,5 Many splinting methods and materials have been described, including suture splints, direct resin splints, wire-composite splints, nylon-monofilament-composite splints, polyethylene fibre-reinforced splints, orthodontic splints and titanium trauma splints.6-8
Wire-composite splinting has become the gold standard because of its simplicity, the availability of materials and a track record of successful outcomes.5 Wire-composite splints commonly use stainless steel wires, which are flexible, have no memory and can be passively adapted to fit the teeth.8 Although orthodontic splinting has been suggested, evidence of the efficacy of orthodontic appliances in managing dental trauma,9 especially complex trauma, is lacking.
In this case report, we describe the use of a fixed orthodontic appliance to manage complex dental trauma in a pediatric patient after failure of a conventional wire-composite splint.
Case Report
Diagnosis
A 7-year-old boy presented to a private dental practice after sustaining severe orofacial trauma 2 weeks earlier. A wire-composite splint that had been constructed by a pediatric dentist following the injury was failing (Fig. 1). At the time of injury, no manual repositioning had been undertaken. As the wire-composite splint began to debond, the patient’s mother sought a second opinion from a general dentist, who deemed the teeth unsalvageable because of their persistent mobility and the failure to facilitate stabilization and periodontal healing. The dentist recommended that teeth 12, 11 and 22 be extracted and prosthetic treatment be deferred for the future. Dissatisfied with this treatment plan, the patient’s mother sought treatment from another pediatric dentist, the corresponding author.
Clinical examination revealed that the patient was in the early mixed dentition stage. His medical history was non-contributory. The boy had sustained severe trauma as well as a periodontal degloving injury to the maxillary permanent incisors. The right maxillary lateral incisor (tooth 12) was severely extruded (about 5 mm) and displaced lingually; it displayed M3 mobility and was traumatically occluding on the mandibular incisors. The right maxillary central incisor (tooth 11) was intruded approximately 4 mm and luxated laterally with its apex perforating the fractured buccal cortical plate; it also had an enamel fracture on the incisal edge. Tooth 11 had not passively reerupted since the trauma. The left maxillary central incisor (tooth 21) had been avulsed and could not be located at the time of injury. The left maxillary lateral incisor (tooth 22) was subluxated and displayed M2 mobility.
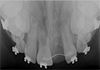
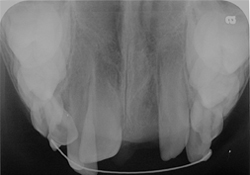
Clinically, all of the traumatized teeth were vital, asymptomatic and responded to thermal stimuli. Radiographic examination revealed that the traumatized teeth were in an early stage of root development; roots were less than half their final length and apices were open. No signs of intraosseous or pulpal pathology were found (Fig. 2).
NOTE: Click to enlarge images.
Figure 1a) and b): Failing wire-composite splint used to treat severe complex dental trauma sustained by a 7-year-old boy.
Treatment
Considering the severe consequences of premature tooth loss, it was decided that every effort should be made to maintain the traumatized teeth. Given the failed attempt at constructing a satisfactory wire-composite splint and the urgent need to stabilize and reposition the teeth, a fixed orthodontic appliance was used as a trauma splint. This allowed for simultaneous management of the various luxation injuries and facilitated future rehabilitation.
The first step was to reopen the wound, debride the granulation tissue and provide primary closure using simple interdental sutures to facilitate soft tissue healing. No teeth were manually repositioned. Further, the patient was prescribed a 0.12% chlorhexidine mouth rinse and instructed to use it in the morning and at night and also to brush the traumatized area gently with a toothbrush dipped in chlorhexidine. The patient was prescribed amoxicillin, 250 mg 3 times a day for 7 days. These preventive measures were critical to minimize the bacterial load in the periodontium, prevent the development of infection and promote healing.10
An orthodontic splint was constructed by bonding 0.018” by 0.022” preadjusted edgewise brackets (Opti-MIM, Cerum Ortho Organizers, Calgary, AB) to the traumatized permanent incisors, the primary canines and the primary second molars (Fig. 3). For convenience, the primary first molars were not included. Notably, the positions of the brackets on teeth 12, 11 and 22 were not ideal; they were simply placed as gently and atraumatically as possible without displacing the teeth or gingiva. Other brackets from other manufacturers with slightly different prescriptions would have worked equally well.
Figure 3a) and b): Orthodontic splint constructed using buccal tubes on the primary second molars, edgewise brackets on the primary canines and traumatized permanent incisors, and a 0.015” coaxial stainless steel wire.
Initially, a 0.015” coaxial stainless steel wire was chosen as the splint wire for several reasons:
- Its extreme flexibility allowed for easy manipulation and placement in the brackets without the need for manual repositioning even with severely malpositioned teeth11
- It was mostly passive with very light forces (stabilizing the teeth with minimal orthodontic movement)11
- No wire bending was necessary 11
This arch wire would gradually bring tooth 12 out of traumatic occlusion and into the arch and would assist in the eruption and repositioning of teeth 11 and 22. Using this technique, adequate stabilization of all the traumatized teeth was achieved, and there was no need to open the bite to relieve the traumatic occlusion on the lingually displaced tooth 12.
The patient was discharged with follow-up appointments scheduled for 1 week, 1 month, 4 months, 7 months, 8 months, 13 months and 19 months. At each appointment, the orthodontic splint was found to be sound, in place and adequately stabilizing each of the traumatized teeth. Vitality was assessed at each visit, radiographs were obtained based on clinical findings and wires were changed. Over the course of treatment, periodontal healing progressed well, the traumatized teeth survived and root and alveolar development continued. None of the traumatized teeth exhibited loss of vitality, excessive mobility or ankylosis. Rather, physiological mobility of each tooth was regained and maintained. Although the overall prognosis has improved significantly, continued long-term follow up is essential, as late-healing complications may occur years after the injury.12
At 7 months after the injury, the arch form had been significantly reestablished (Fig. 4). Tooth 12 had been slightly intruded, repositioned back into the arch and relieved from traumatic occlusion; tooth 11 had been moderately extruded and repositioned lingually. Further, the fractured cortical bone buccal to tooth 11 showed signs of healing as mobility of the segment had returned to normal when assessed with the wire removed. Thus, the teeth had realigned without manual repositioning. Radiographic examination revealed continued root development and healthy bone levels, no signs of pulpal or periradicular pathology and no signs of pulpal calcification (Fig. 5).
Figure 4a) and b): At 7 months 19 days post-trauma, clinical examination shows preservation of all traumatized teeth and significant reestablishment of the arch form.
With the teeth and periodontium stabilized and healing, rehabilitation of the dentition could be carried out. At 7 months, the brackets on teeth 12, 11 and 22 were repositioned ideally, and a sequence of thermal nickel–titanium wires was placed to further level and align the dentition. At 8 months after the sequential wire changes, a 0.016” x 0.022“ rectangular nickel–titanium wire was inserted along with a bracketed pontic to replace tooth 21 and prevent possible drift of teeth 11 and 22 into the edentulous space (Fig. 6). The fractured incisal edge of tooth 11 was also repaired with composite resin.
An occlusal radiograph taken 13 months post-injury showed incomplete root development in tooth 11, likely secondary to the intrusion injury, which could affect the long-term prognosis (Fig. 7). However, there were no signs of pulpal or periradicular pathology or pulpal calcification in any of the traumatized teeth, and healthy bone levels in the region of the trauma were observed. A ligature wire was bonded to the lingual surfaces of teeth 11 and 22 to prevent movement of the pontic.
At the last follow-up visit, 19 months after the initial trauma, all of the involved teeth were clinically asymptomatic and vital with physiological mobility. At this point, the brackets were removed, and a Hawley retainer with a pontic to replace the missing tooth 21 was inserted for space maintenance and esthetics during transition of the dentition (Fig. 8). The patient was scheduled for regular visits, with a second round of fixed comprehensive orthodontic treatment to be considered if necessary to achieve ideal occlusion of the teeth before prosthodontic rehabilitation.
Discussion
Flexible, passive splints, such as wire-composite splints, are recommended in the guidelines for treatment of traumatic injuries to the dentition because of their proven track record. However, the management of dental trauma is not conducive to one-size-fits-all solutions. As demonstrated in this case, orthodontic splinting may provide distinct advantages over conventional techniques.
Gentle Slow Repositioning of Teeth by Light Continuous Force vs. Manual Traumatic Repositioning: Orthodontic splinting may negate the need for manual repositioning of traumatized teeth as it gradually repositions the teeth over time. Teeth with open apices display a profound capacity for revascularization after trauma.13 However, manual repositioning involves a great force producing a secondary trauma to the already traumatized tooth, potentially causing further damage to the periodontal ligament and the neurovascular bundle and jeopardizing the vitality of the teeth. Gradual repositioning is a less traumatic alternative that may safeguard tooth vitality, prevent ankylosis and encourage periodontal healing, especially in a healthy growing child.
Splinting of Severely Malpositioned Teeth: Orthodontic splinting allows for stabilization of severely malpositioned teeth through the use of flexible wires. Thus, complex injuries, in which teeth are displaced in different directions, can be effectively managed.
Ease of Fabrication: Construction of an orthodontic splint is an atraumatic, simple, quick procedure that does not require any specialized training.14 As shown in this case, wire bending, composite manipulation and ideal bracket placement at the time of the injury may not be possible or required. General dentists, pediatric dentists and orthodontists who are comfortable with tooth movement and dealing with trauma can provide such treatment.
Ease of Evaluation and Adjustment: Orthodontic splinting allows for effortless clinical evaluation of the traumatized teeth, as the wire can simply be removed to evaluate mobility and periodontal healing. Further, wires and the position of brackets can be easily changed depending on rate of recovery and changes in treatment objectives.
Preservation of Physiological Mobility: Orthodontic splints have been shown to be non-rigid and able to maintain physiological mobility.9 These splints can be maintained for prolonged periods; in this case, the brackets and wire were maintained in their original position for 7 months without ankylosis, replacement resorption or other adverse effects. Further, the application of light orthodontic forces on immature teeth has little effect on tooth development and final root length.15
Ease of Rehabilitation: Orthodontic splinting allows for gradual reestablishment, and even possible improvement, of the arch form after traumatic injury to the teeth. This facilitates future rehabilitation of both avulsed and displaced teeth as the teeth may be moved orthodontically after healing is complete.
Despite these benefits, there are few reports on the efficacy of orthodontic bonded brackets in managing dental trauma. Andreasen and colleagues13,16 have shown that orthodontic splinting after trauma is associated with an increased degree of pulp canal obliteration compared with wire-composite splinting. However, these studies were retrospective reviews of hospital reports on dental trauma in which the splinting technique involved orthodontic bands cemented on each traumatized tooth and fixed with acrylic resin. This has limited applicability in the current scenario as it uses an outdated orthodontic technique. The complications observed may have been a direct result of the excessive forces applied during banding and cementing — a technique that has long been replaced by acid-etch bonding, brackets and flexible wires. Moreover, Andreasen states that orthodontic band/acrylic fixation was used only on intruded teeth and, thus, the results may be biased as intruded teeth have the worst prognosis in terms of pulp survival after trauma.12
Several other studies have suggested that orthodontic splints should be used with caution as it is difficult to construct a passive splint that does not exert force on the teeth.5,17 Forces from the orthodontic splint could disrupt the healing process in traumatized teeth and lead to unwanted tooth movement. However, neither of these complications was experienced in our case, and successful healing was observed. A recent study9 also reports that orthodontic splinting has been used successfully to treat intrusion injuries and has been associated with superior outcomes compared with both passive re-eruption and manual repositioning in terms of tooth loss and complications.
Treatment Considerations: There are 4 main situations in which an orthodontic splint may be advantageous:
- When it is not possible to construct an adequate wire-composite splint, e.g., in the case of severely malpositioned teeth
- When multiple dental injuries must be addressed complicating the splint design
- When repositioning of the traumatized teeth is required, e.g., intrusive luxation
- When the least traumatic method of repositioning is desirable to safeguard pulpal vitality, e.g., in the case of teeth with open apices, which have greater potential for pulpal revascularization
Orthodontic splinting is a simple and versatile procedure. The following general principles should guide the construction of an orthodontic splint:
- Forces should be as light as possible to establish a splinting effect
- Adequate anchorage should be established using non-traumatized posterior teeth
- Optimal oral hygiene is critical for quick healing without complications
- The patient should be monitored consistently to manage potential complications and monitor the movement of teeth
Conclusions
Orthodontic splinting should to be considered as a viable, first choice for managing severe dental trauma in the pediatric population.
THE AUTHORS
References
- Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: a review of the literature. Aust Dent J. 2000;45(1):2-9.
- Andreasen JO, Andreasen FM, Andersson L, editors. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Oxford: Wiley-Blackwell; 2007.
- von Arx T. Splinting of traumatized teeth with focus on adhesive techniques. J Calif Dent Assoc. 2005;33(5):409-14.
- Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, et al. Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Dental Traumatology. 2007;23(2):66-71.
- Oikarinen K. Tooth splinting: a review of the literature and consideration of the versatility of a wire-composite splint. Endod Dent Traumatol. 1990;6(6):237-50.
- Filippi A, von Arx T, Lussi A. Comfort and discomfort of dental trauma splints — a comparison of a new device (TTS) with three commonly used splinting techniques. Dental Traumatology. 2002;18(5):275-80.
- 7. Andreasen JO, Bakland LK, Flores MT, Andreasen FM, Andersson L. Traumatic dental injuries, 3rd ed. Oxford: Wiley-Blackwell; 2011.
- Kwan SC, Johnson JD, Cohenca N. The effect of splint material and thickness on tooth mobility after extraction and replantation using a human cadaveric model. Dent Traumatol. 2012;28(4):277-81. Epub 2011 Nov 23.
- Chaushu S, Shapira J, Heling I, Becker A. Emergency orthodontic treatment after the traumatic intrusive luxation of maxillary incisors. Am J Orthod Dentofacial Orthop. 2004;126(2):162-72.
- Hammarström L, Blomlöf L, Feiglin B, Andersson L, Lindskog S. Replantation of teeth and antibiotic treatment. Endod Dent Traumatol. 1986;2(2):51-7.
- Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. Mosby; 2007.
- Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth — the development of pulp necrosis. Endod Dent Traumatol. 1985;1(6):207-20.
- Andreasen FM. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod Dent Traumatol. 1989;5(3):111-31.
- Mackie IC, Warren VN. Dental trauma: 3. Splinting, displacement injuries, and root fracture of immature permanent incisor teeth. Dent Update. 1988;15(8):332-5.
- Mavragani M, Bøe OE, Wisth PJ, Selvig KA. Changes in root length during orthodontic treatment: advantages for immature teeth. Eur J Orthod. 2002;24(1):91-7.
- Andreasen FM, Zhijie Y, Thomsen BL, Andersen PK. Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endod Dent Traumatol. 1987;3(3):103-15.
- Prevost J, Louis JP, Vadot J, Granjon Y. A study of forces originating from orthodontic appliances for splinting of teeth. Endod Dent Traumatol. 1994;10(4):179-84.
|
Gallery of all Figures in article |
|||||
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|











-2010-01.jpg)