Body
Loosened Dental Implant Associated with Pain
- Clinically, loosening of a dental implant is characterized by increased mobility with or without pain. (Fig. 1)
- Radiographically, the loss of peri-implant crestal bone is associated with loose implants.
- Loosening of a dental implant soon after placement is primarily due to surgical trauma, overheating of the osteotomy, complicated wound healing, insufficient primary stability and/or initial overload. Intermediate or late loosening of a dental implant more commonly results from marginal infection (peri-implant mucositis) and/or biomechanical overload, influenced largely by host characteristics.
- Loose dental implants could also be the result of surgical trauma due to overheating of the osteotomy or nonideal implant position resulting in nonaxial forces during occlusion, improper crown design, high occlusal alignment or improper size selection of the implant and abutment.
- Loose dental implants can also result from implant surface characteristics and/or designs.
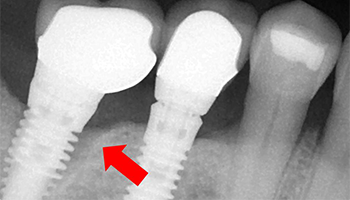 Figure 1. Radiolucency around the cervical portion (arrow) of the implant associated with clinical mobility and gingival inflammation.
Figure 1. Radiolucency around the cervical portion (arrow) of the implant associated with clinical mobility and gingival inflammation.
Presentation
Population
- Individuals with poor oral hygiene, parafunctional habits, bruxism and high occlusal loading.
- Patients at risk for loosened dental implants include heavy smokers; individuals with poorly controlled diabetes, osteoporosis, or osteomalacia; individuals taking certain medications; and those who have previously undergone irradiation of the implant site.
- Patients with peri-implantitis (inflammation of the tissues surrounding the implant). Peri-implant mucositis affects the gingiva and is usually reversible. If untreated, this may progress to marginal peri-implantitis that manifests as progressive bone loss around the implant and may result in implant mobility if untreated.
Signs
- Mobility of the prosthesis/implant.
- Implant/prosthesis may no longer be in the mouth.
- Pain on percussion.
- Clinically observable bone loss around the implant.
- Gingivitis if associated with peri-implantitis: bleeding on probing, increased pocket depth.
- Uncontrolled exudates if associated with an underlying infection.
- Varying degrees of bone loss around the implant appears as peri-implant radiolucency, which usually measures more than half of the length of the implant.
Symptoms
- Pain on function.
- Mobility of the prosthesis/implant.
Investigation
- Obtain a thorough medical history.
- Perform intra- and extraoral examinations to establish the cause of the loose dental implant. In some iatrogenic cases this might be challenging.
- Obtain periapical radiographs to confirm the clinical investigations.
Diagnosis
Based on clinical mobility and radiographic peri-implant radiolucency, a diagnosis of implant failure can be established.
Notes
- Radiographic assessment alone may be misleading; radiological bone loss may not always be associated with dental implant mobility. Therefore, clinical investigation is crucial to establishing the diagnosis.
- Careful clinical assessment should reveal a mobile implant. The diagnosis may be more difficult under a multiple-unit fixed partial denture (FPD) and might require removal of the overlying prosthesis to identify the mobile implant.
Differential Diagnosis
Carefully examine the implant and the prosthesis to differentiate between a loose prosthesis and the body of the implant.
Treatment
- In the case of a loose dental implant, the only treatment is to immediately remove all components of the implant to avoid the progressive destruction of the surrounding tissues. A "wait-and-watch" technique or splinting must not be used.
- The difficulty of implant removal might depend on the severity of mobility and the prosthetic components over the implant. For example a very loose implant under a single-unit fixed partial prosthesis is easier to remove than a slightly mobile implant under a 3-unit fixed partial prosthesis.
- After a careful investigation of the clinical situation, the general practitioner must decide whether to carry out the implant removal or refer the patient to a specialist.
Common Initial Treatment
- Management of the patient's psychological and functional discomfort is crucial to successful treatment of the complication:
- Prescribe analgesics to reduce pain after removal of implant.
- Inform the patient of the diagnosis and etiology of the failed implant, if identifiable. Discuss future treatment options with the patient. This may include immediate replacement with another implant of greater dimensions if the implant site is suitable or guided bone regeneration followed by placement of a new implant.
- Inform the patient about the need for a new prosthesis over the implants.
Removing the implant
- A mobile implant may easily be removed by rotating it counter-clockwise. Rotation with minimal luxation reduces trauma and damage to the surrounding bone and soft tissue. Use of a driver, counter-torque ratchet or forceps may help implant removal. If the implant has strong soft tissue attachments, local anesthesia should be administered to reduce discomfort to the patient.
-
If the implant supports a multiple-unit FPD, the prosthetic components over the failed implant will need to be removed.
- For an FPD that has been screwed in, remove the restorative material from the screw channel and unscrew the FPD.
- For an FPD that has been cemented, drill through the FPD with a bur or carefully tap it out using a pneumatic crown remover while making sure not to cause trauma to the adjacent implants.
- Removal of the implant may vary according to the implant system and design. For example, an external hex implant would require an adaptor if a counter-torque ratchet is being used for removal.
- Granulation tissue, if any, should be carefully removed before further treatment.
Referral to a Specialist
- If you decide not to remove the implant or if the implant is not easy to remove, refer the patient to a periodontist or an oral and maxillofacial surgeon.
- Remove the prosthesis or relieve the occlusion to avoid any lateral forces on the implant that may cause further damage to the implant site before the implant can be removed.
THE AUTHORS
Suggested Readings
- Pommer B, Frantal S, Willer J, Posch M, Watzek G, Tepper G. Impact of dental implant length on early failure rates: a meta-analysis of observational studies. J Clin Periodontol. 2011;38(9):856-63.
- Ashle ET, Covington LL, Bishop BG, Breault LG. Ailing and failing endosseous dental implants: a literature review. J Contemp Dent Pract. 2003;4(2): 35-50.
- Baqain ZH, Moqbel WY, Sawair FA. Early dental implant failure: risk factors. Br J Oral Maxillofac Surg. 2012;50(3):239-43.
- Sakka S, Baroudi K, Nassani MZ. Factors associated with early and late failure of dental implants. J Investig Clin Dent. 2012;3(4):258-61.
- Hsu YT, Fu JH, Al-Hezaimi K, Wang HL. Biomechanical implant treatment complications: a systematic review of clinical studies of implants with at least 1 year of functional loading. Int J Oral Maxillofac Implants 2012;27(4):894-904.
- Babbush CA, editor. Dental Implants: Principles and Practice. Philadeplphia: W.B. Saunders Company; 1991.
- Misch CE. Contemporary Implant Dentistry. Missouri: Mosby Elsevier; 2007.
- Froum SJ, editor. Dental Implant Complications: Etiology, Prevention, and Treatment. Oxford: Wiley-Blackwell; 2010.



