Up to 47% of North American adults experience some form of periodontal disease1-3 and, as our population ages, this prevalence is predicted to increase.4 This will not only affect health care costs for the individual patient, but will also increase the economic burden on the population as a whole. A recent global burden of disease study,5 although heterogeneous in terms of case definitions of periodontitis, noted that severe periodontitis was the sixth most prevalent condition in the world, with prevalence increasing steeply between the third and fourth decades of life.
Recent progress in periodontal research has increased our understanding of etiopathogenesis and treatment options. Still, one of the biggest challenges is to develop methods to detect periodontitis (and peri-implantitis) at the earliest stages. Although early diagnosis increases the chance of intervention before irreversible destruction of the periodontium occurs,6 diagnosis remains a challenge because of the multifactorial nature of the disease.7
Clinical examination, including measurement of probing depths, clinical attachment and periodontal recession, together with radiographic analysis of alveolar bone loss, remains the current gold standard. Although general dentists and hygienists are trained to perform these procedures, a recent survey in Nova Scotia, Canada, found that only 37.8% perform full-mouth probing and 43.3% take selective probing depth measurements.8 Similarly, a survey of dental practitioners in Victoria, Australia,9 reported that, although most dentists are confident in their ability to recognize advanced periodontal disease, only 40% carry out full mouth probing. Further, although most respondents to a survey of Scottish dental practitioners10 were confident in diagnosing periodontal disease, only 40% were confident in treating it. Lack of consistency among general practitioners in terms of diagnosis and treatment may play a key role in the under-diagnosis of periodontal disease at early stages.
The specialty of periodontics includes the diagnosis, treatment and maintenance of healthy, functional attachment levels around teeth and implants.11 Most patients receive prophylactic periodontal therapy in general practice and referral to a specialist may be reserved for cases of unresolved progression of disease or more advanced or aggressive diseases. Because periodontics is a referral-based specialty, understanding the dynamics of referral patterns from general dentists is critical to the viability of the periodontal practice within the community. However, our perspective on these referral patterns has been mainly that of general dentists.8-10,12,13
In addition to treatment and prevention of the effects of periodontal destruction, patients may also be referred to periodontists for plastic (mucogingival) surgery, pre-prosthetic surgery, hard and soft tissue augmentation and dental implants. However, to date, there is no information about the types of procedures performed in periodontal practices across Canada or the patterns of referral from general dentists. The purpose of this project is to examine the profile of periodontal practices in terms of services provided and referral patterns. Data from this survey may guide the development of pre- and post-doctoral dental curricula. This study may also increase awareness of periodontics as a specialty and serve as a reference point for evaluating future trends.
Methods
Questionnaire
An online cross-sectional survey was developed, consisting of 3 sections: demographics, referral dynamics and periodontal procedures performed. It was tested for content and face validity with a convenience sample of 5 academic and clinical periodontists. The final questionnaire consisted of 45 questions and was formatted on Opinio, an online survey system offered by Information Technology Services, Dalhousie University.
Questions included multiple choice (both single and multiple answers); rating, ranking and matrix of choices (1 answer per row); open-ended numerical textboxes; and comment/essay boxes. In the periodontal procedure section, a Likert scale was used; it consisted of 5 categories based on frequency of procedures performed: never, rare, occasionally, often and very often.
Hidden conditions were programmed into the questionnaire to allow respondents, who met specific criteria, to answer specific questions. For example, if a respondent had worked for 10 years or more and noted changes in referral pattern, he or she would be asked about the type of changes noted. Similarly, if a respondent performed certain procedures, such as sinus lift or grafting, he or she would be asked for details. For all other respondents, these questions would not be visible.
Participants
The sampling frame consisted of all active members of the Canadian Academy of Periodontology (CAP) (n = 280). Participants were excluded if they were students, international or military members. The Health Sciences Research Ethics Board at Dalhousie University granted ethics approval for the project (REB#2013-3124).
Figure 1: Protocol for survey. Reminders were sent only to non-respondents. Only the participant codes were known to the primary investigator to track response. (Note: as responses were not mandatory, number of respondents varied) 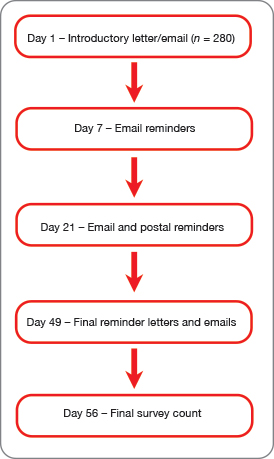
Survey Application
A mixed-mode approach was used to contact participants (Fig. 1). On day 1, an introductory letter was sent by email and post to 280 active Canadian periodontists. On day 7, email-only reminders were sent. On day 21, reminders where sent by both email and post. On day 49, final email and postal reminders were sent, and, on day 56, access to the online survey was closed.
All participants were given instructions for accessing the online survey and a unique code for logging in. Participants were advised that their participation was voluntary, that informed consent was implied by completion of the survey and that all responses were confidential and anonymous. An incentive was provided for completing the survey: a chance to win a Surface RT tablet (Microsoft, Redmond, Wash., USA).
A code sheet linked the names and addresses of participants with their assigned unique codes. This allowed us to send reminders to non-respondents and those with incomplete surveys only. The code sheet was accessible only to the administrative assistant at CAP's head office, who provided the list of codes to investigators as needed. The names of participants were blinded to the investigators.
Statistical Analyses
Statistical analysis was performed using SPSS v. 20. Both descriptive and inferential analyses were performed.
To analyze the frequency of procedures, the Likert scale was collapsed in 2 ways: in a binary variable, "yes" (which included rarely, occasionally, often and very often) or "no" (never) and a 3-category variable, "frequently" (often and very often), "infrequently" (rarely and occasionally) and "never" (never). The latter was used to ascertain how often procedures were performed in a private periodontal office.
Using backward stepwise (Wald) regression, we compared the effect of the covariables "age" (< 45 years or ≥ 45 years), "year of graduation" (before or after 1990), "years in active practice" (< 20 years or ≥ 20 years) and "sex") on binary variables (yes/no) for laser use, single implants, intravenous sedation and sinus lifts. A p value of < 0.05 was deemed statistically significant.
Results
Of the 280 potential respondents, 164 started the survey online (58.6%); 135 completed the entire survey and 151 answered most questions. Response rates by days 7, 21 and 49 were 16.4%, 38.2% and 41%, respectively, with a cumulative final response rate of 58.6% by day 56.
| Demographic | Respondents | |
|---|---|---|
| No. | % | |
| Note: ABP = American Board of Periodontology, FRCDC = Fellow of the Royal College of Dentists of Canada. As responses were not mandatory, number of respondents varied. | ||
| Age (n = 141) | ||
| < 35 | 21 | 14.9 |
| 35–44 | 25 | 17.7 |
| 45–54 | 43 | 30.5 |
| 55–64 | 42 | 29.8 |
| ≥ 65 | 10 | 7.1 |
| Sex (n = 141) | ||
| Male | 104 | 73.8 |
| Female | 34 | 24.1 |
| Prefer not to disclose | 3 | 2.1 |
| Years in practice (n = 138) | ||
| < 10 | 44 | 31.9 |
| 10–19 | 33 | 23.9 |
| 20–29 | 39 | 28.3 |
| ≥ 30 | 22 | 15.9 |
| Year of graduation (n = 138) | ||
| Before 1980 | 8 | 5.8 |
| 1980–1989 | 37 | 26.8 |
| 1990–1999 | 41 | 29.7 |
| 2000–2009 | 31 | 22.5 |
| 2010 or later | 21 | 15.2 |
| Professional designations (n = 134) | ||
| FRCDC | 73 | 54.5 |
| Diplomat of ABP | 29 | 21.6 |
| Neither | 47 | 35.1 |
| Other | 15 | 11.2 |
Demographics
Not all respondents answered all questions, so the number of respondents varied. Most respondents 103/139 (74.1%) were full-time private practitioners. The male to female ratio was 3:1. Ages ranged from < 35 years (14.9%) to > 65 years (7.1%), with the highest proportion of respondents in the 45–54 year age group (30.5%) (Table 1). Of the respondents, 44/139 (31.9%) had been in active practice < 10 years and 94/139 (68.1%) for ≥ 10 years; 15.9% had been in practice for > 30 years. Year of graduation was similarly distributed. A majority of respondents 102/134 (76.1%;) held either Fellowship in the Royal College of Dentists of Canada (FRCDC) or were a Diplomate of the American Board of Periodontology (ABP), while the rest held neither of these designations or had other designations including Member of the Royal College of Dentists of Canada, Fellow of the International Team of Implantology, Fellow of the International College of Dentistry and Fellow of the American College of Dentistry. Almost all respondents who graduated after 1999 held the FRCDC designation, alone or in combination with the ABP credential (Table 1).
Representative of the Canadian demographic, most respondents were from Ontario 50/141 (35.5%;), followed by Quebec 29/141 (20.6%;), British Columbia 26/141 (18.5%), Alberta 16/141 (11.6%), Nova Scotia 8/141 (5.7%;), Manitoba 6/141 (4.3%;), New Brunswick 3/141 (2.1%;), Newfoundland and Labrador 1/141 (0.7%;), Prince Edward Island 1/141 (0.7%;) and Saskatchewan 1/141 (0.7%). No CAP-registered periodontists live in the Northwest Territories, Nunavut or Yukon.
On average, the respondents saw 13 patients a day, of which 3 were new patients. In a typical week, respondents spent, on average, 3.5 h reading periodicals related to periodontics. This reading material was most frequently the Journal of Periodontology (94.8%), followed by the International Journal of Periodontics and Restorative Dentistry (49.6%) and the International Journal of Oral and Maxillofacial Implants (40.0%). Among the Internet sources frequently used for information regarding periodontal practice, the most common was the American Academy of Periodontology (AAP) website (84.6%), followed by the CAP website (33.8%) and provincial dental association websites (16.2%).
In a typical year, respondents (n=141)attended 3 professional conferences. The most frequently attended conferences were national association conferences, (e.g., AAP, CAP ) (96.4% ), followed by those focused on implants (70.3%) and periodontal-restorative themes (39.9%).
Referral Dynamics
Among Canadian periodontists who had practised 10 or more years and noticed a change in referral pattern in the last 10 years (94/138 or 68.1% of respondents), most 65/105 (61.9%) noted a decrease in the number of referrals (Fig. 2). Of patients referred from general dentists, those seeking limited treatment were the most frequent 106/148 (71.6%). "Limited treatment" is often referred to as prescription surgery and would include crown lengthening and mucogingival procedures, for example, but not management of patients with periodontal diseases. Most respondents 103/138 (74.6%) felt that patients were being referred later in their disease progression compared with 10 years ago.
On an average, 40 new patients a month were referred to a periodontal practice. Of those referred specifically for periodontal disease, most had generalized periodontitis (56.1%), followed by mucogingival disease without active periodontitis (26.3%) and localized periodontitis (15.5%).
Initial examination of newly referred patients revealed that most had 1–4 missing teeth (63.9%); 1–4 teeth were planned for extraction or given a hopeless prognosis (85.0%). Almost all new referrals had private dental insurance (95.2%), although some had public insurance (social services, provincial/federal plans) (2.7%) and others had no dental insurance (2.1%).
Procedures
Non-surgical therapy: Scaling and root planing (debridement) are the basis of periodontal therapy and these procedures are often completed by periodontists themselves (in addition to their hygienists). We also evaluated frequency of other non-surgical services, including photodynamic therapy, management of temporomandibular disorders and occlusal therapies (Fig. 3). Most periodontists 125/140 (89.3%;) perform occlusal therapies; common procedures include bite plane therapy 80/119 (67.2%), periodontal splinting 62/119 (52.1%,), major occlusal adjustment 53/119 (44.5%,) and minor occlusal adjustment 25/ 119 (21.0%,).
Figure 2: A) and B) Changes in number (n=105) and timing (n=105) received from general dentists as perceived by respondents who noted changes in the pattern over the last 10 years. C) Types of referrals in the past month (n=148) 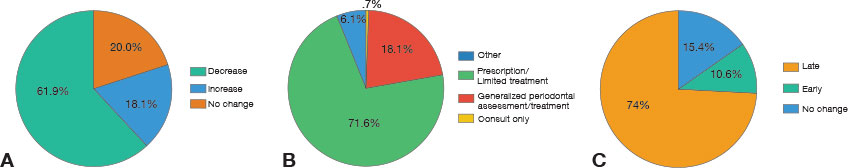
Figure 3: Frequency of use of non-surgical therapies by respondents. 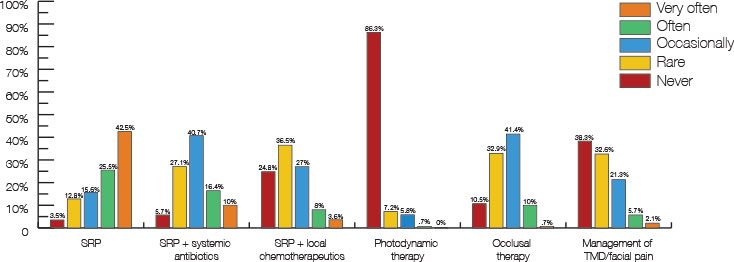 Scaling and root planing (SRP) n= 141; SRP + systemic antiboitics n=140; SRP + Local chemotherapy n=137; Photodynamic therapy n=139; Occlusal therapy n=140; Temporomandibular dysfunction (TMD)/facial pain n=141.
Scaling and root planing (SRP) n= 141; SRP + systemic antiboitics n=140; SRP + Local chemotherapy n=137; Photodynamic therapy n=139; Occlusal therapy n=140; Temporomandibular dysfunction (TMD)/facial pain n=141.
Surgical therapy: All respondents performed surgical management of periodontitis with varying frequencies (Table 2), including open flap debridement, pre-restorative crown lengthening, esthetic crown lengthening and connective tissue grafts.
Implant therapy: The frequency of implant-related procedures is shown in Table 2. Single implant placement was more likely to be placed by respondents with < 20 years in practice (p = 0.036), who graduated before 1990 (p = 0.024) and who were < 45 years old (p = 0.031) (Table 3). No difference was noted between sexes (p = 0.862). Regression analysis suggested that years in practice may be a predictor for single implant placement; however, the model did not reach statistical significance (odds ratio [OR]= 4.8; p = 0.056).
Sinus lift: Most respondents performed sinus lifts, and almost half (43.3%) performed them frequently. More respondents used the indirect approach (osteotome, socket approach) than the direct approach (lateral window) (74.1% vs. 66.7%); however, the difference was not statistically significant (p > 0.05). χ2 analysis revealed that periodontists in practice < 20 years and those < 45 years of age performed sinus lift more frequently (p = 0.042 and p = 0.048, respectively) (Table 3). Regression analysis showed that years in practice (< 20 years: OR=6.5, p = 0.005) and sex (males: OR=6.5, p = 0.007) were predictors of performing sinus lifts.
Intravenous and oral sedation: The oral route was the most popular sedation method among respondents: 54/141 (38.3%) used it frequently and 52.5% infrequently. Intravenous sedation was performed more frequently by those with < 20 years of active practice (p = 0.005) and those who graduated in 1990 or later (p = 0.048) (Table 3). Regression analysis showed that only years in practice (< 20 years) was significantly related to the use of intravenous sedation (OR =4.9, p = 0.001).
Lasers: Most respondents never used lasers in their office 98/141 (69.5%); of those 14.2% used them frequently. Of those who used lasers, the most popular choice was Nd:Yag (75%), followed by diode (33.3%) and CO2 (30.8%). Laser use was more frequent among male periodontists (35.9%) compared with females (14.7%), and the difference was significant (χ2: p = 0.020; Table 3). Regression analysis showed a significant relation between being male and laser use (OR 4.0, p = 0.015).
| Category | Procedure | No. of respondents | Frequency performed (%) | ||
|---|---|---|---|---|---|
| Never | Infrequently | Frequently | |||
| Periodontal surgery | Gingivectomy | 140 | 2.9 | 87.8 | 9.3 |
| Flap procedure (with or without resective osseous) | 142 | 0 | 21.1 | 78.9 | |
| Crown lengthening (pre-restorative) | 141 | 0 | 24.1 | 75.9 | |
| Guided tissue regeneration | 142 | 2.1 | 40.2 | 57.7 | |
| Periodontal plastic surgery | Free gingival grafts | 140 | 7.9 | 30.0 | 62.1 |
| Connective tissue graft (autogenous) | 141 | 0.0 | 11.3 | 88.7 | |
| Gingival grafts using allograft | 142 | 25.4 | 56.4 | 18.2 | |
| Esthetic crown lengthening | 141 | 0 | 55.4 | 44.6 | |
| Implant therapy | Single implant placement | 142 | 6.3 | 12 | 81.7 |
| Implant placement in esthetic zone | 142 | 6.3 | 14.1 | 79.6 | |
| Treatment of ailing implant(s) | 142 | 3.6 | 69.5 | 26.9 | |
| Removal of failed implant(s) | 142 | 10.6 | 81.7 | 7.7 | |
| Covariable | Single implant (%) | p | Sinus lift (%) | p | IV sedation (%) | p | Laser use (%) | p |
|---|---|---|---|---|---|---|---|---|
| *Significant difference (p < 0.05). Note: IV = intravenous. |
||||||||
| Years in practice | n=138 | n=137 | n=135 | n=137 | ||||
| < 20 years | 97.4 | 0.036* | 49.6 | 0.042* | 36.8 | 0.005* | 29.9 | 0.844 |
| ≥ 20 years | 88.5 | 32.8 | 15.3 | 28.3 | ||||
| Year of graduation | n=138 | n=137 | n=135 | n=137 | ||||
| Before 1990 | 86.7 | 0.024* | 75.0 | 0.113 | 16.3 | 0.048 | 31.8 | 0.643 |
| 1990 or later | 95.8 | 86.0 | 32.6 | 28.0 | ||||
| Sex | n=138 | n=137 | n=136 | n=137 | ||||
| Male | 93.3 | 0.862 | 84.5 | 0.152 | 28.4 | 0.825 | 35.9 | 0.020* |
| Female | 94.1 | 73.5 | 26.5 | 14.7 | ||||
| Age | n=141 | n=140 | n=138 | n=140 | ||||
| < 45 years | 100.0 | 0.031* | 91.3 | 0.048* | 35.6 | 0.186 | 32.6 | 0.638 |
| ≥ 45 years | 90.5 | 77.7 | 24.7 | 28.7 | ||||
Discussion
The design of this protocol was inspired by a review of physician surveys presented at the American Association for Public Opinion Research (AAPOR) conference in 2008.14 Although electronic surveys of health professionals have typically resulted in low response rates compared with postal surveys,15-17 mixed-mode designs have increased response rates.14,18 Our response rate of 53.9% is significant, compared with rates across other national surveys (23.1% for Patel and colleagues19 and 37.3% for Tingey and colleagues20) and confirms the effectiveness of combining an electronic questionnaire with email and postal reminders when surveying dental professionals.
Our survey also demonstrates good external validity, in that our sample represents about 70% of all periodontists in Canada and the response rate was moderately high. Recall bias can affect the collection of accurate data21-23; however, our questionnaire did not ask respondents to recall specific numbers or details of procedures; they were asked about the frequency of procedures performed within the last month. This short time for recall is likely to provide accurate information.24
Most respondents were periodontists in full-time private practice. The large proportion of responses from Ontario, Quebec and British Columbia is likely because of the large metropolitan areas in these provinces. As a referral specialty, dense pockets of population, where the dentist to population ratio is high, can serve as attractive niches.
There was a marked increase in FRCDC and ABP designations among those graduating after 1999. In the late 1990s, the Royal College of Dentists of Canada together with the provincial dental regulatory authorities, established a task force that concluded that all dental specialist candidates must pass the National Dental Specialty Examination to obtain a licence as a specialist in their province starting in January 2001.25 This policy likely caused candidates to apply for Fellowship in addition to their specialty licence and, hence, the increase in designation noted in the results of our survey.
In terms of referral patterns, a decrease in the overall number of referrals, delayed timing of referrals with respect to disease progression and limited referral types were noted by most respondents who had been in practice more than 10 years. This change in referral dynamics could have implications for the treatment options provided by periodontists. Generally, a goal of periodontal therapy is to prevent tooth loss.26-28 The decision to extract teeth is guided not only by initial assessment, but also by severity of periodontal disease, furcation involvement, etiologic factors, restorative factors, smoking status, systemic condition and clinician's skills.29 An initially unfavourable prognosis can be converted to a favorable long-term prognosis30 with appropriate periodontal management; however, delaying referral often means that patients have lost tooth supporting tissue, and the only predictable and viable option may be extraction. Thus, timing of referral and intervention with proper treatment is crucial.
With the advent of implant therapy and bone regeneration procedures, the consequences of missing teeth or a hopeless prognosis may not be as catastrophic as they once were.31-33 Dental implants are among the most common procedures performed in a periodontal practice. With the increasing prevalence of implant placement, there is potential for an increase in adverse effects, such as peri-implant mucositis or peri-implantitis.6 As specialists, periodontists are often called on to treat ailing or failing supporting structures around implants. Our survey showed that a quarter of periodontists treat ailing implants "frequently" and 1 in 12 removes failed implants. These data provide a baseline to explore future trends, as anectodal evidence suggests that with more dentists placing implants, the number of ailing and failing implants may increase.
Canadian periodontists frequently perform traditional surgical procedures such as flap debridement and crown lengthening. Although these can be considered the "bread-and-butter" of private periodontal practice, periodontics residency training should reflect the demands of the dental community and the changing dynamics between generalists and specialists. Training in sinus lift procedures, intravenous sedation and advanced regenerative/grafting procedures, could increase the repertoire of the specialist and augment the periodontics–restorative management of patients.34
Of those respondents who performed sinus lifts, more used an indirect rather than a direct approach; however, the difference was not significant. The direct approach has been shown to result in a significantly greater gain in bone height compared with the crestal approach (8.4 vs. 4.4 mm), although the sample size was small in this study.35 No difference in implant success rate could be found. As such, both approaches are options to be used as the situation demands. Further insight can be gained by examining graduate programs to determine which types of procedure are taught and how instructor influence affects practice philosophy of residents.
In a telephone survey of 1101 Canadians, 68.2% said they preferred sedation or general anesthesia for periodontal surgery, compared with 46.5% who preferred sedation or general anesthesia for tooth extractions.36 It appears that training in intravenous sedation is a relatively recent phenomenon, as its use was more popular among respondents with fewer than 20 years in active practice compared with those in practice longer. Similarly, more recent graduates were more likely to use intravenous sedation. In the United States, almost half the periodontists who responded to a postal survey offered intravenous sedation in their practices.20 Although our results show that less than a third of respondents offer intravenous sedation, this difference may be due to biased sampling, as the response rate in the US study was low.
Laser therapy is an ongoing controversial issue among many specialists. From an evidence-based perspective, the AAP claims that lasers provide no additional benefit over traditional scaling and root planing for sulcular/pocket debridement.37 Most periodontists in our survey had never used lasers (69.5%) or performed photodynamic therapy (86.3%). The greater popularity of laser use among male compares with female periodontists may be because men are more "technology driven"; however, the relevance of this result remains questionable. A survey of 102 North American graduate periodontics programs found that about half used lasers in their training and a third used lasers in 10 or fewer patients.38 The same study expressed concern over the lack of laser training in graduate programs and the potential impact in the private practice setting where commercial training may prove inadequate for novice clinicians. It appears that most of our respondents were in agreement with the lack of scientific evidence on laser use in clinical settings, as reflected by the infrequent use of lasers reported in our survey.
Conclusion
A mixed-mode survey method using both electronic and postal reminders is an efficient way to attain a high response rate when surveying dental professionals. In summary, recent graduates were more likely to perform sinus lift procedures and use intravenous sedation. Male periodontists were more likely to use lasers and do sinus lifts than females. Among respondents who saw changes in the last 10 years, most noted an overall decrease in the number and timing of referrals for management of periodontal disease and more referrals for limited treatment.
THE AUTHORS
References
- Eke PI, Dye B, Wei L, Slade G, Thornton-Evans, G, Borgnakke W et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol 2015;86(5):611-22
- Summary Report of the findings of the Oral Health Component of the Canadian Health Measures Survey 2007–2009. Ottawa: Health Canada; 2010.
- Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ, CDC Periodontal Disease Surveillance workgroup. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914-20.
- Brown LJ, John BA, Wall TP. The economics of periodontal disease. Periodontol 2000. 2002;29:223-34.
- Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 2014;93(11):1045-53.
- Slots J. Periodontology: past, present, perspectives. Periodontol 2000. 2013;62(1):7-19.
- Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction. Periodontol 2000. 1997;14:9-11.
- Ghiabi E, Weerasinghe S. The periodontal examination profile of general dentists in Nova Scotia, Canada. J Periodontol. 2011;82(1):33-40.
- Darby IB, Angkasa F, Duong C, Ho D, Legudi S, Pham K, et al. Factors influencing the diagnosis and treatment of periodontal disease by dental practitioners in Victoria. Aust Dent J. 2005;50(1):37-41.
- Chestnutt IG, Kinane DF. Factors influencing the diagnosis and management of periodontal disease by general dental practitioners. Br Dent J. 1997;183(9):319-24.
- hat is a periodontist? Ottawa: Canadian Academy of Periodontology; 2016. Accessed 2015 Mar 23. Available: http://www.cap-acp.ca/en/public/periodontist.html.
- Linden GJ, Stevenson M, Burke FJ. Variation in periodontal referral in 2 regions in the UK. J Clin Periodontol. 1999;26(9):590-5.
- McGuire MK, Scheyer ET. A referral-based periodontal practice — yesterday, today, and tomorrow. J Periodontol. 2003;74(10):1542-4.
- Flanigan TS, McFarlane E, Cook S. Conducting survey research among physicians and other medical professionals — a review of current literature. In Proceedings of the American Association for Public Opinion Research 63rd Annual Conference. Oakbrook Terrace, Ill.: AAPOR; 2008. pp. 4136-47.
- Akl E, Maroun N, Klocke RA, Montori V, Schünemann HJ. Electronic mail was not better than postal mail for surveying residents and faculty. J Clin Epidemiol. 2005;58(4):425-9.
- Losh ME, Thompson N, Lutz G. The effect of mode on response rates and data quality in a survey of physicians. In Proceedings of the American Association for Public Opinion Research 59th Annual Conference. Oakbrook Terrace, Ill.: AAPOR; 2004.
- McMahon SR, Iwamoto M, Massoudi MS, Yusuf HR, Stevenson JM, David F, et al. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics. 2003;111(4 Pt 1):e299-303.
- Beebe TJ, Stoner SM, Anderson KJ, Williams AR. Selected questionnaire size and color combinations were significantly related to mailed survey response rates. J Clin Epidemiol. 2007;60(11):1184-9.
- Patel AM, Blanchard SB, Christen AG, Bandy RW, Romito LM. A survey of United States periodontists' knowledge, attitudes, and behaviors related to tobacco-cessation interventions. J Periodontol. 2011;82(3):367-76.
- Tingey BT, Clark SH, Humbert LA, Tingey JD, Kummet CM. Use of intravenous sedation in periodontal practice: a national survey. J Periodontol. 2012;83(7):830-5.
- Bradburn NM, Rips LJ, Shevell SK. Answering autobiographical questions: the impact of memory and inference on surveys. Science. 1987;236(4798):157-61.
- Grimes DA, Schulz KF. Bias and causal association in observational research. Lancet. 2002;359(9302):248-52.
- Hassan E. Recall bias can be a threat to retrospective and prospective research designs. Internet J Epidemiol. 2005;3(2).
- Margetts BM, Vorster HH, Venter CS. Evidence-based nutrition — the impact of information and selection bias on the interpretation of individual studies. S Afr J Clin Nutr. 2003;16(3):78-87.
- Kennedy DB. The Royal College of Dentists of Canada: history, misconceptions and recent developments. J Can Dent Assoc. 2001;67(10):574-6.
- Oliver RC. Tooth loss with and without periodontal therapy. Periodont Abstr. 1969;17(1):8-9.
- Lindhe J, Nyman S. Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol. 1984;11(8):504-14.
- Oliver RC, Brown LJ. Periodontal diseases and tooth loss. Periodontol 2000. 1993;2:117-27.
- Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91.
- Greenstein G, Greenstein B, Cavallaro J. Prerequisite for treatment planning implant dentistry: periodontal prognostication of compromised teeth. Compend Contin Educ Dent. 2007;28(8):436-46; quiz 447, 470.
- Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155-70.
- Yi SW, Ericsson I, Kim CK, Carlsson GE, Nilner K. Implant-supported fixed prostheses for the rehabilitation of periodontally compromised dentitions: a 3-year prospective clinical study. Clin Implant Dent Relat Res. 2001;3(3):125-34.
- Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res. 2007;18(6):669-79.
- Accreditation requirements for periodontics programs (updated Nov. 2013). Ottawa: Commission on Dental Accreditation of Canada; 2013. [accessed 2015 Mar 30]. Available: www.cda-adc.ca/cdacweb/en/accreditation_requirements/dental_specialties/
- Pal US, Sharma NK, Singh RK, Mahammad S, Mehrotra D, Singh N, et al. Direct vs. indirect sinus lift procedure: a comparison. Nat J Maxillofac Surg. 2012;3(1):31-7.
- Chanpong B, Haas DA, Locker D. Need and demand for sedation or general anesthesia in dentistry: a national survey of the Canadian population. Anesth Prog. 2005;52(1):3-11.
- American Academy of Periodontology statement on the efficacy of lasers in the non-surgical treatment of inflammatory periodontal disease. J Periodontol. 2011;82(4):513-4.
- Ghiabi E, Taylor KL. Teaching methods and surgical training in North American graduate periodontics programs: exploring the landscape. J Dent Educ. 2010;74(6):618-27.



