The mandibular premolars are located close to the mental foramina (Fig. 1). As such, various events affecting these teeth, such as odontogenic infection1 and orthodontic, endodontic, periodontal or surgical misadventure, may result in neurosensory disturbance of the mental nerves.2-4 In one retrospective study, the incidence of mental paresthesia resulting from periapical infection or pathology was 0.96%. In another 0.24% of cases in the same study, mental paresthesia was a complication of root canal treatment (caused by severe overfill in one case and iatrogenic perforation of mechanical instrumentation through the root and into the mental nerve in the second case).1 The incidence of mental paresthesia resulting from orthodontic, periodontal and surgical misadventure cannot be determined but is presumably low, as most such cases have been reported as individual case reports.
In endodontology, elimination of infection from the pulp and dentin followed by adequate intracanal preparation and proper sealing constitute the basic principles of root canal treatment. Ideally, mechanical preparation and filling should be limited to the root canal, as overinstrumentation or extrusion of chemical fillings beyond the apical foramen to the adjacent nerve may give rise to neurosensory disturbances such as anesthesia, paresthesia or dysesthesia.5 Unfortunately, cases of endodontic extrusion of various filling or irrigation agents continue to be reported, despite recent advances in endodontology.
Neurosensory Disturbance in Relation to the Premolars
Neurosensory disturbance caused by dental diseases or procedures, as described above, occurs because of the close proximity of the mandibular premolars (especially the second bicuspid) to the mental foramina (Fig. 2). To avoid causing such disturbance during dental procedures, the practitioner must be aware of the location of the mental foramina, for example, by palpation or radiography. However, the mental foramen may not be evident with routine periapical radiography if it is below the margin of the film.
 Figure 1: Three-dimensional computed tomography scan showing the relationship
between the premolar teeth and the mental foramen.
Figure 1: Three-dimensional computed tomography scan showing the relationship
between the premolar teeth and the mental foramen.
 Figure 2: Panoramic radiograph showing the relationship between the mental
foramina and the mandibular premolars.
Figure 2: Panoramic radiograph showing the relationship between the mental
foramina and the mandibular premolars.
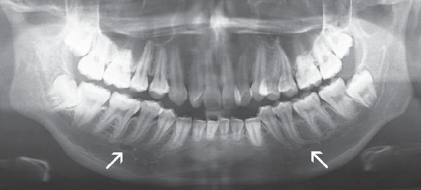 Figure 3: Panoramic radiograph showing bilateral
mental foramina at the apex of the mandibular second premolars.
The appearance mimics that of a periapical lesion.
Figure 3: Panoramic radiograph showing bilateral
mental foramina at the apex of the mandibular second premolars.
The appearance mimics that of a periapical lesion.
Each mental foramen may be located anywhere between the first and second premolars, and the prevalence of cases in which the mandibular premolars are located very close to the mental foramen (Fig. 3) has been reported. For example, Fishel and colleagues,6 on the basis of a radiographic study, reported that the mental foramina were located at the apices of the first premolars in 15.4% of patients and at the apices of the second premolars in 13.9% of patients. In another study, performed at the current author's institution, researchers examining the relationship of the second premolars to the mental foramina found that the foramina were located at the apices of the second premolars in slightly more than one-third of patients (unpublished data). In addition, the visibility of the mental foramina was significantly limited in women and in patients 50 years of age or older (unpublished data).
In their morphometric study, Phillips and colleagues7 reported that each mental foramen was located an average distance of 2.18 mm mesially and 2.4 mm inferiorly from the radiographic apex of the second premolar. More precisely, each mental foramen was found to be located, on average, anywhere between 3.8 mm mesial, 2.7 mm distal, 3.4 mm above or 3.5 mm below the apex of the respective second premolar. In contrast, the apex of each second premolar was between 0 and 4.7 mm from the respective mental foramen in various cadaveric studies.1,8
Given this variability in the location of the foramen relative to the apex, it seems that there is no "absolute safety zone" in the premolar region where damage to the mental nerve can be avoided if the accidental extrusion of endodontic files and materials occurs. It must also be borne in mind that the studies and measurements described above involved patients with normal mandibles (i.e., without pathosis). The presence of apical periodontitis resulting in destruction of bone or the presence of a radicular lesion, such as a cyst, would further erode the bone that protects the mental nerve.
Clinical Implications
In the clinical setting, if the apical seat is not well prepared or the apex is not completely formed, it is easy to extrude a small-diameter file or any irrigation or filling materials beyond the apex. The first premolars seem to have sufficient space to compensate for such an error, as they are usually located further away from the mental foramina. Even so, it should be remembered that as many as 15.4% of mental foramina are located at the apical level of the first premolars.6 Therefore, each case must be assessed individually. If the dentist suspects close proximity of these structures, it is suggested that 2 periapical radiographs, at different angles (parallax technique), be obtained to ascertain the exact relationship of the premolars to the mental foramina. The presence of a via falsa and a large periradicular cyst should be ruled out by periapical radiographs before any endodontic treatment is started. The routine use of a good apex locator will also help to avoid extrusion of files beyond the apex.
Dentists fulfill their obligation to protect patients from harm by ensuring a good understanding of the proximity of the mental foramina to the premolar teeth before undertaking any treatment in this region of the mouth.
THE AUTHOR
References
- Knowles KI, Jergenson MA, Howard JH. Paresthesia associated with endodontic treatment of mandibular premolars. J Endod. 2003;29(11):768-70.
- Baxmann M. Mental paresthesia and orthodontic treatment. Angle Orthod. 2006;76(3):533-7.
- Scarano A, Di Carlo F, Quaranta A, Piattelli A. Injury of the inferior alveolar nerve after overfilling of the root canal with endodontic cement: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(1):e56-9.
- Pogrel MA, Thamby S. The etiology of altered sensation in the inferior alveolar, lingual, and mental nerves as a result of dental treatment. J Calif Dent Assoc. 1999;27(7):531, 534-8.
- Pogrel MA. Damage to the inferior alveolar nerve as the result of root canal therapy. J Am Dent Assoc. 2007;138(1):65-9.
- Fishel D, Buchner A, Hershkowith A, Kaffe I. Roentgenologic study of the mental foramen. Oral Surg Oral Med Oral Pathol. 1976;41(5):682-6.
- Phillips JL, Weller RN, Kulild JC. The mental foramen: 2. Radiographic position in relation to the mandibular second premolar. J Endod. 1992;18(6):271-4.
- Denio D, Torabinejad M, Bakland LK. Anatomical relationship of the mandibular canal to its surrounding structures in mature mandibles. J Endod. 1992;18(4):161-5.
