| ABSTRACT | Download PDF of Article |
Patient supplement on dry mouth |
Patients with xerostomia, or dry mouth, resulting from various causes, are at higher risk for developing caries because of a loss of saliva and its benefits. A loss of saliva increases the acidity of the mouth, which affects many factors that contribute to the development of caries, such as proliferation of acid-producing bacteria, inability to buffer the acid produced by bacteria or from ingested foods, loss of minerals from tooth surfaces and inability to replenish the lost minerals, and loss of lubrication. Currently, a number of new products that can substitute for these functions of saliva or induce production of saliva are available in Canada. Some of these products are reviewed and a protocol for caries prevention in this high-risk population is proposed.
Introduction
Maintaining the oral health of patients with salivary gland dysfunction or hypofunction can be challenging for dental practitioners and patients. These patients commonly complain of xerostomia, the subjective sensation of dry mouth, which can cause considerable distress. In addition, patients with insufficient saliva may also suffer from increased risk of oral infections, a higher rate of caries, increased dental expenses and decreased quality of life.
Decreased salivary flow most commonly occurs as an adverse effect of medications, but is also associated with head and neck radiation, psychological affective disorders, systemic diseases, including diabetes, and HIV infection, and less frequently with graft-versus-host disease. It can also occur as part of autoimmune disorders, including lupus, scleroderma and Sjögren syndrome.
Functions of saliva include the development of dental pellicle, a film that forms on tooth enamel and protects against mineral loss from the tooth surface; replenishment of tooth surface minerals such as calcium and phosphate; the provision of antibacterial activity and buffering activity, which keeps oral pH neutral; and mechanical removal of residual food particles from the teeth.1,2
As a result of the development of new products, an aggressive approach to caries management can now minimize the damage to the dentition associated with the lack of saliva. The dental health care provider can choose from a variety of commercial products that can be incorporated into a patient-specific treatment plan as needed, depending on the degree of loss of salivary flow. Some of these new products are outlined below.
Remineralization of Teeth
A lack of saliva exposes the teeth to acidic challenges from food and drinks, as well as to the acid produced by acidogenic bacteria. Saliva acts as a reservoir for the calcium and phosphate ions needed to remineralize the tooth surface. Acids dissolve calcium and phosphate ions from the enamel in a process called demineralization,1 which can eventually lead to cavities. The loss of salivary buffering capacity may cause oral pH to become acidic. As the pH falls below 5.5, demineralization occurs.
Various lipids, glycoproteins and proteins contained in saliva also deposit onto the tooth surface to form dental pellicle.2 Dental pellicle acts as a selectively permeable barrier to calcium and phosphate ions, but not to acids, and aids in the prevention of demineralization and in the remineralization of teeth.3 Pellicle also protects teeth from acid challenges by preventing direct contact between the acids and the enamel.
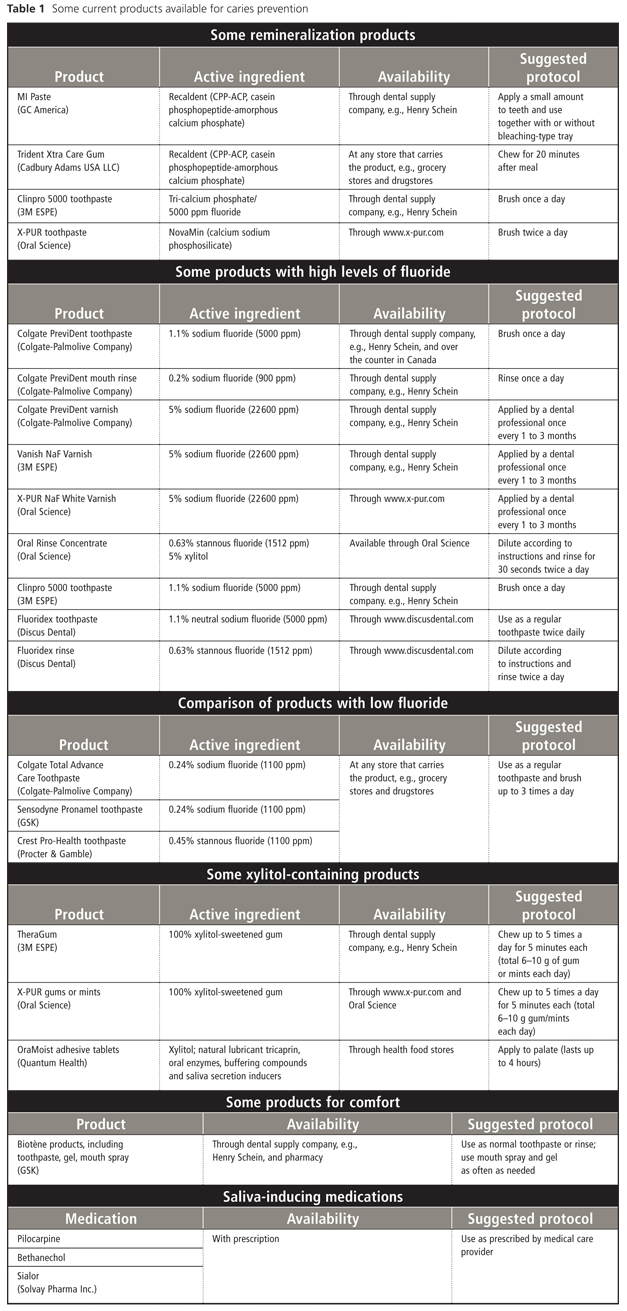
In a dry mouth, natural remineralization and protection may not occur because of the lack of salivary calcium and phosphate ions. To compensate, alternative sources are required. Many new remineralizing products have been developed, including MI Paste (GC America, Alsip, IL), Clinpro 5000 toothpaste (3M ESPE, London, ON), and X-PUR toothpaste (Oral Science, Longueuil, QC). Each contains different remineralizing compounds (Table 1).
MI Paste contains a compound called Recaldent, which is also a component of Trident Xtra Care Gum (Cadbury Adams USA LLC, Parsippany, NJ). Recaldent, or casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), increases the number of available calcium and phosphate ions that help remineralize the enamel. The presence of casein phosphopeptide, a peptide derivative of casein, stabilizes amorphous calcium phosphate, a compound of soluble salts of calcium and phosphate, which allows more ions to reach the enamel.4
Applying a small amount of MI Paste directly to the teeth, as well as chewing Recaldent-containing gum, can help reduce the rate of demineralization.4,5 MI Paste is safe for use by lactose-intolerant patients, but is contraindicated for patients with casein (milk-protein) allergies. MI Paste can be applied to tooth surfaces with a fingertip or wet cotton swab after brushing. Brush application of MI Paste is discouraged because it may not be as effective. Medication carrier trays can be used for longer exposure, similar to the application of fluoride gels. Because MI Paste does not contain fluoride, its overnight application in medication carriers is well tolerated.
The remineralizing ingredient of the new product Clinpro 5000 toothpaste is tricalcium phosphate, which consists of calcium oxides, calcium phosphate and free phosphates. This product contains a high concentration (5000 ppm) of fluoride, which also aids in remineralization by attracting calcium and phosphate ions to the tooth's surface.1 Clinpro 5000 is applied as a toothpaste and is not suitable for overnight use because of its high fluoride concentration.
The active ingredient in another new remineralizing product, X-PUR toothpaste, is NovaMin, or calcium sodium phosphosilicate. The sodium ions help to increase oral pH and decrease acidity in the mouth. Calcium sodium phosphosilicate forms a layer on the tooth surface that is structurally similar to natural enamel. X-PUR is recommended as a toothpaste application, but can also be used in medication carriers for longer exposure because, like MI Paste, it does not contain fluoride.
Fluoride
Fluoride treatment reduces the formation of caries in several ways. Fluoride decreases demineralization by reducing the solubility of enamel and increases remineralization by attracting calcium and phosphate ions to the tooth's surface. Fluoride can inhibit the enzyme enolaze that is required for the metabolism of bacterial carbohydrates, thus reducing the concentration of bacteria in the mouth.1
Fluoride is available in many forms, including varnish, rinse, toothpaste and gel. The daily use of fluoride rinses and toothpastes, combined with fluoride varnish applied up to once every 3 months by a dental team,6 is recommended for patients with dry mouth.
Although regular use of low fluoride-containing dentifrices (most over-the-counter products contain < 1500 ppm) effectively reduces caries,7 products containing higher concentrations of fluoride are preferred for high-risk patients. Patients are often deterred by the high price of high-potency fluoride products. Counselling by the dentist or hygienist about the potential savings in dental costs can promote compliance with prescribed regimens.
Colgate's PreviDent (Colgate-Palmolive Co., New York, NY) products contain high concentrations of sodium fluoride (NaF). These include a dentifrice with 1.1% NaF (5000 ppm), mouth rinse with 0.2% NaF (900 ppm), and varnish with 5% NaF (22 600 ppm). Many of the products are available to dental offices from dental supply companies. In Canada, PreviDent 5000 Plus toothpaste is also available over the counter.
Clinpro 5000, which contains 1.1% NaF, may have the added benefit of providing tricalcium phosphate for the remineralization of teeth.
Fluoridex toothpaste (Discus Dental, Culver City, CA) contains 1.1% NaF (5000 ppm) and Fluoridex rinse contains 0.63% stannous fluoride (approximately 1512 ppm of fluoride). All high fluoride-containing products are available to dental offices whose staff can then dispense these items to their patients.
Other high fluoride-containing products include Vanish NaF White Varnish (3M ESPE) and X-PUR NaF White Varnish (Oral Science). Both contain 5% NaF (approximately 22 600 ppm). Varnish can be applied up to once every 3 months for high-risk populations or up to once monthly for patients with severe dry mouth.
X-PUR Oral Rinse Concentrate from Oral Science, which was released at the end of 2010, contains 0.63% stannous fluoride (approximately 1512 ppm of fluoride), together with 5% xylitol, a naturally occurring sweetener that controls acid-producing bacteria.
Although fluoride has an important role in preventing caries, overuse of fluoride can result in fluorosis in some cases.8 Therefore, patients should be checked for signs and symptoms of fluorosis when placed on a high-fluoride regimen and for compliance with the prescribed regimen.
Bacteria and Caries
Acidogenic (acid-producing) bacteria are generally found in a normal mouth, along with other bacteria, and are kept in balance through various interactions among the different species. When food is ingested, acid-producing bacteria ferment the carbohydrates to produce lactic acid, which decreases oral pH. Normally, the buffering capacity of saliva helps to neutralize the acid produced. However, in a dry mouth, the natural buffering capacity is lost and the mouth becomes more acidic, which predisposes it to acid-producing bacteria.9
Streptococcus mutans and Lactobacillus are acidogenic bacteria that are major contributors to the formation of dental caries. The levels of these bacteria are higher in patients with hyposalivation.10-12 Because dietary sucrose promotes the growth of cariogenic bacteria,13 maintaining a low-sugar diet is an effective way to decrease the number of acid-producing bacteria. The use of xylitol, a naturally occurring sugar alcohol, to replace other sugars effectively controls the number of acid-producing bacteria.
Xylitol, a common sweetener, is a natural 5-carbon alcohol sugar that cannot be fermented by bacteria. It is noncariogenic because it inhibits the formation of caries by reducing the amount of acid produced by acidogenic bacteria.14,15 For dry mouth, patients should chew xylitol-containing gum or mints up to 5 times a day for about 5 minutes each time (2–3 g of gum or mints each time). Products with 100% xylitol are most effective for reaching this target. Excess intake may produce osmotic diarrhea.16
Some xylitol-containing products include TheraGum (3M ESPE), X-PUR gums and mints (Oral Science), all of which contain 100% xylitol. Quantum Health's OraMoist (Quantum Inc., Eugene, OR) adhesive tablet, which adheres to the palate for up to 4 hours as it slowly dissolves and can be used while sleeping, also contains some xylitol, as well as a natural lubricant tricaprin, oral enzymes, buffering compounds and saliva-secretion inducers to help moisten the mouth.
Other approaches to reduce cariogenic bacteria include the use of chlorhexidine, which has been shown to decrease the levels of Streptococci mutans when applied as a rinse, gel or varnish. However, S. mutans levels usually return to pretreated states within months when treated with a chlorhexidine rinse.17 The effect of chlorhexidine varnish has been inconclusive: some studies18-20 show significant reduction of caries with the use of 10% chlorhexidine-containing varnish. A decrease in S. mutans levels may not translate into a decrease in caries because of other contributing factors to its formation, including diet, the ability to produce saliva and oral-hygiene practices. Use of chlorhexidine is, therefore, not recommended as the sole method of preventing caries for patients with dry mouth; chlorhexidine should be used in combination with other treatments. Another option, Prevora, a varnish containing 10% chlorhexidine acetate, from CHX Technologies Inc. (Toronto, ON), can be used in conjunction with fluoride treatment as a part of caries prevention for this high-risk population.
Dietary Changes
Since dietary sugars promote acid production by acidogenic bacteria and since caries results from acidic attacks on tooth surfaces, a diet low in sugar and acidic drinks is recommended for those at increased risk of caries because of the lack of saliva to buffer the pH of the mouth. Replacing sugar with sweeteners such as xylitol and sugary or acid drinks with water can reduce the available fermentable sugars and decrease acid production by bacteria.
Salivary Flow and Oral Comfort
For patients with hyposaliva, the lack of saliva not only increases the risk of caries, but also creates an uncomfortable sensation of dryness. Oral products to treat dry mouth from Biotène (GSK, London, UK), which include toothpaste, mouthwash with antibacterial enzymes, mouth spray and liquid, are helpful for relieving the discomfort of xerostomia.
For some patients, chewing gum can also help to increase salivary flow and increase mouth comfort. For patients who are able to chew gum, gums containing 100% xylitol are ideal since xylitol cannot be fermented by acid-producing bacteria, so it helps prevent caries.
Use of parasympathetic drugs, such as pilocarpine, bethanechol and the cholagogue anethole trithione (Sialor, Solvay Pharma Inc., ON), to stimulate salivary production in those with residual salivary-gland function can help relieve oral dryness.21-24 Although these agents are effective sialogogues in patients with intact salivary glands, their efficacy is reduced in patients with changes in their salivary glands that are secondary to radiation or disease. In addition, concomitant disease states, drug interactions and adverse effects can limit their usefulness.
Tooth Brushing
Plaque is formed when bacteria bind to the enamel. For patients with hyposalivation, the plaque contains more acid-producing bacteria than normal, putting these patients at higher risk for acid challenges and consequent formation of caries. Because of their higher risk, these patients should brush their teeth carefully 2 or 3 times a day with either a manual toothbrush or an electric toothbrush with an oscillating and rotating head for optimal removal of plaque.25,26 Waterpik (Water Pik, Inc., Fort Collins, CO) is also a tool that can be used to remove plaque, especially for those who may have difficulties using dental floss because of irritation and bleeding. However, the use of a Waterpik for treating dry mouth is not clear.27 Therefore, its use should be dependent solely on patient preference. Good dental hygiene is important for preventing caries by removing bacteria-containing plaque and residual food particles.
Studies of Natural Products for Preventing Caries
Although many existing products help prevent dental caries, few natural products have been tested in vivo. Most studies of the use of natural products as agents for preventing caries examined the effects of these products on the inhibition of bacterial activity. Many of the studies found at least some inhibition of the development of caries in vitro with the use of naturally occurring compounds such as tea extract, Chinese herb extract, grape seed extract, and compounds of Amur grape leaf and stem.28-33 Although all of these compounds show promising results for reducing caries and reducing caries-causing bacteria, more and better studies are required, especially for high-risk patients and those with dry mouth.
Suggested Protocol for Preventing Caries
A lack of saliva and loss of many functions render most single-product groups inadequate for controlling caries. Combination therapy, however, may prove very effective. A typical protocol might include the following:
- using remineralization paste and chewing gum containing Recaldent to replenish calcium and phosphate ions
- using high-fluoride varnish once every 1 to 3 months to reduce the susceptibility of enamel to acid challenges
- using high-fluoride-containing toothpaste and rinse daily, with monitoring for signs of fluorosis and patient compliance
- chewing xylitol gum up to 5 times a day for 5 minutes each time to reduce acid production by bacteria, and increase saliva and oral comfort
- taking medications, including pilocarpine, bethanechol or Sialor, to induce salivary flow and increase comfort for those with residual salivary gland function
- using products made by Biotène for comfort and possible antibacterial activities
- brushing teeth carefully to remove any plaque and residual food particles with either a manual brush or an electric brush with an oscillating and rotating head, and possibly using a Waterpik to replace floss, as patients prefer
- changing to a diet low in sugar and acidic drinks
- potentially using chlorhexidine in conjunction with these other procedures
In our clinical practice, we often ask a patient to sleep with a remineralizing agent (e.g., MI Paste, X-Pur) in medication carriers fabricated like bleaching trays to extend exposure to the agent to keep the mouth wetter at night and to provide a mechanical barrier to an acidic environment.
Because no studies that directly compare the effectiveness of these new products are available, patient preference plays an important role in determining which products and procedures can be easily incorporated into a daily home care routine, and which offer the best relief for the symptoms of dry mouth.
THE AUTHORS
References
- Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc. 2000;131(7):887-99.
- Edgar WM, O'Mullane DM. The role of saliva in demineralization and remineralization of teeth. In: Saliva and dental health. 1st ed. Plymouth: British Dental Association; 1990. p. 19-24.
- Hara AT, Ando M, Gonzalez-Cabezas C, Cury J, Serra MC, Zero DT. Protective effect of the dental pellicle against erosive challenges in situ. J Dent Res. 2006;85(7):612-6.
- Llena C, Forner L, Baca P. Anticariogenicity of casein phosphopeptide-amorphous calcium phosphate: a review of the literature. J Contemp Dent Pract. 2009;10(3):1-9.
- Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. Caries Res. 2004;38(6):551-6.
- American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137(8):1151-9.
- Lynch RJ, Navada R, Walia R. Low-levels of fluoride in plaque and saliva and their effects on the demineralisation and remineralisation of enamel; role of fluoride toothpastes. Int Dent J. 2004;54(5 Suppl 1):304-9.
- Eichmiller FC, Eidelman N, Carey CM. Controlling the fluoride dosage in a patient with compromised salivary function. J Am Dent Assoc. 2005;136(1):67-70.
- Marsh PD. Dental plaque as a biofilm and a microbial community — implications for health and disease. BMC Oral Health. 2006;6(Suppl 1):S14.
- Almstahl A, Wikstrom M, Kroneld U. Microflora in oral ecosystems in primary Sjögren's syndrome. J Rheumatol. 2001;28(5):1007-13.
- Eliasson L, Carlen A, Almstahl A, Wikstrom M, Lingstrom P. Dental plaque pH and micro-organisms during hyposalivation. J Dent Res. 2006;85(4):334-8.
- Almstahl A, Wikstrom M, Stenberg I, Jakobsson A, Fagerberg-Mohlin B. Oral microbiota associated with hyposalivation of different origins. Oral Microbiol Immunol. 2003;18(1):1-8.
- Paes Leme AF, Koo H, Bellato CM, Bedi G, Cury JA. The role of sucrose in cariogenic dental biofilm formation — new insight. J Dent Res. 2006;85(10):878-87.
- Kakuta H, Iwami Y, Mayanagi H, Takahashi N. Xylitol inhibition of acid production and growth of mutans Streptococci in the presence of various dietary sugars under strictly anaerobic conditions. Caries Res. 2003;37(6):404-9.
- Roberts MC, Riedy CA, Coldwell SE, Nagahama S, Judge K, Lam M, et al. How xylitol-containing products affect cariogenic bacteria. J Am Dent Assoc. 2002;133(4):435-41.
- Scientific Opinion of the Panel on Dietetic Products, Nutrition and Allergies on a request from LEAF Int, Leaf Holland and Leaf Suomi Oy on the scientific substantiation of a health claim related to xylitol chewing gum/pastilles and reduction of the risk of tooth decay. The EFSA Journal 2008;852:1-16. Available: www.efsa.europa.eu/en/efsajournal/doc/852.pdf (accessed 2011 June 22).
- Autio-Gold J. The role of chlorhexidine in caries prevention. Oper Dent. 2008;33(6):710-6.
- Ashley P. Effectiveness of chlorhexidine varnish for preventing caries uncertain. Evid Based Dent. 2010;11(4):108.
- Twetman S. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res. 2004;38(3):223-9.
- Banting DW, Papas A, Clark DC, Proskin HM, Schultz M, Perry R. The effectiveness of 10% chlorhexidine varnish treatment on dental caries incidence in adults with dry mouth. Gerodontology. 2000;17(2):67-76
- Chainani-Wu N, Gorsky M, Mayer P, Bostrom A, Epstein JB, Silveman S Jr. Assessment of the use of sialogogues in the clinical management of patients with xerostomia. Spec Care Dentist. 2006;26(4):164-70.
- Berk L. Systemic pilocarpine for treatment of xerostomia. Expert Opin Drug Metab Toxicol. 2008;4(10):1333-40.
- Nusair S, Rubinow A. The use of oral pilocarpine in xerostomia and Sjögren's syndrome. Semin Arthritis Rheum. 1999;28(6):360-7.
- Hamada T, Nakane T, Kimura T, Arisawa K, Yoneda K, Yamamoto T, et al. Treatment of xerostomia with the bile secretion-stimulating drug anethole trithione: a clinical trial. Am J Med Sci. 1999;318(3):146-51.
- Deery C, Heanue M, Deacon S, Robinson PG, Walmsley AD, Worthington H, et al. The effectiveness of manual versus powered toothbrushes for dental health: a systemic review. J Dent. 2004;32(2):197-211.
- He T, Biesbrock AR, Walters PA, Bartizek RD. A comparative clinical study of the plaque removal efficacy of an oscillating/rotating power toothbrush and an ultrasonic toothbrush. J Clin Dent. 2008;19(4):138-42.
- Jahn CA. The dental water jet: a historical review of the literature. J Dent Hyg. 2010;84(3):114-20. Epub 2010 Jul 5.
- Linke HA, LeGeros RZ. Black tea extract and dental caries formation in hamsters. Int J Food Sci Nutr. 2003;54(1):89-95.
- Ooshima T, Minami T, Aono W, Izumitani A, Sobue S, Fujiwara T, et al. Oolong tea polyphenols inhibit experimental dental caries in SPF rats infected with mutans streptococci. Caries Res. 1993;27(2):124-9.
- Yim N, Ha do T, Trung TN, Kim JP, Lee S, Na M, et al. The antimicrobial activity of compounds from the leaf and stem of Vitis amurensis against two oral pathogens. Bioorg Med Chem Lett. 2010;20(3):1165-8. Epub 2009 Dec 6.
- Li M, Liu Z. In vitro effect of Chinese herb extracts on caries-related bacteria and glucan. J Vet Dent. 2008;25(4):236-9.
- Wu CD. Grape products and oral health. J Nut. 2009;139(9):1818S-23S. Epub 2009 Jul 29.
- Xie Q, Bedran-Russo AK, Wu CD. In vitro remineralization effects of grape seed extract on artificial root caries. J Dent. 2008;36(11):900-6. Epub 2008 Sept 25.
A patient handout about dry mouth has been developed as a supplement to this article. The handout is available at: jcda.ca/article/b85
