Oral candidiasis
Common opportunistic infection from yeast-like organism Candida albicans.
Presentation
Population
- Typically elderly patients
- Infants
- Medically compromised individuals
Signs
- Pseudomembranous: creamy-white soft plaques that can be wiped away to expose an erythematous mucosa (Fig. 1)
- Erythematous: generalized but well-defined atrophic erythematous macules or plaques (Fig. 2)
- Hyperplastic: white areas that cannot be wiped away (Fig. 3)
- Angular cheilitis: fissuring, scaling, and erythema of the corners of the mouth (Fig. 4)
- Median rhomboid glossitis: red or red and white patch of mid dorsum of tongue anterior to the circumvallate papillae (Fig. 5)


Fig. 1: Pseudomembranous candidiasis due to prolonged denture wear (a). Resolution of infection after practising proper denture hygiene and nystatin oral rinse (b).

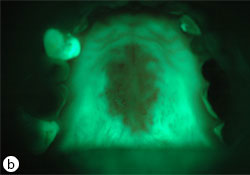

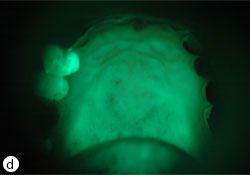
Fig. 2: Erythematous candidiasis due to improper use of steroid inhaler (a). Under autofluorescent light, a diffuse loss of green fluorescent due to tissue inflammation (b). Resolution of infection after preventive measures and clotrimazole 10mg oral troches (c). The green fluorescent re-appear after resolution of infection (d).


Fig. 3: Hyperplastic candidiasis (a) and (b).

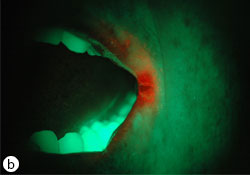

Fig. 4: Angular cheilitis (a). Under autofluorescent light, the orange signal indicates microbial colonization (b). 3 weeks post-topical therapy of clotrimazole 1% cream (c).


Fig. 5: Median rhomboid glossitis (a). 3 weeks after clotrimazole oral troches treatment (b).
Symptoms
- Could be asymptomatic to the patient
- Nonspecific oral sensory changes (i.e., burning, tingling, metallic/foul taste)
Investigation
Identify Possible Etiology
Ask about the patient’s medical/dental history.
- Local factors: prolonged use of prosthetic or orthodontic oral appliances, poor oral hygiene, dry mouth, overclosure of lip
- Systemic factors: immunocompromised state (e.g., Sjögren syndrome, AIDS, uncontrolled diabetes mellitus, other endocrine dysfunctions, malnutrition/malabsorption [e.g., vitamin B deficiency])
- Medical side effects: recent completion of broad-spectrum antibiotics, systemic or local corticosteroids (e.g., asthma inhalers), organ transplant antirejection therapy, chemotherapy
Clinical Investigation
- Cytologic smear samples should be prepared chairside, and then submitted to a laboratory for microscopic diagnosis.
- Tissue biopsy should be performed to rule out other epithelial conditions, if not responsive to antifungal therapy.
Diagnosis
Diagnosis is based on clinical signs and symptoms, in conjunction with exfoliative cytological examination. When exfoliative cytology is not available, clinical response to empirical antifungal medication suggests a retrospective diagnosis of candidiasis.
Differential Diagnosis
Bacterial or viral infection, oral mucositis (e.g., lichenoid mucositis, contact sensitivity, physical/thermal/chemical irritation), oral epithelial (pre-) malignancy.
Treatment
Non-pharmaceutical Management (local treatment)
The objective is to remove or rectify identifiable contributory etiologies to improve the therapeutic outcome and minimize recurrence.
- Denture-wearing patients: Clean the denture and avoid wearing it overnight. Soak the denture in a dilute solution of bleach (1 tsp for 8 oz of water) or in chlorhexidine gluconate 0.12% and rinse thoroughly before reinsertion in the mouth. Caution: The colour of the prosthesis may be altered.
- Dry mouth patients: Ensure adequate hydration and chew xylitol sugar-free gum to improve saliva flow.
- Angular cheilitis patients: Avoid licking the lesions as this will further superinfect them with salivary bacteria. Discard all lip balm or lipstick currently in use to avoid reinoculation with the infectious agent.
- Steroid inhaler users: Brush and rinse the palate after each inhalation. Refer patient to the pharmacist to review the proper aerosol inhalation technique and consider the need for inhaler chamber (spacer) and alternative metered-dose inhaler device, if needed.
Pharmaceutical Management (topical antifungal treatment)
The objective is to enhance the antifungal delivery by prolonging the contact time of the medicine directly to the infective site. Topical treatment is usually required for at least 2 weeks to eradicate the infection, although patients might feel symptom resolution 3–4 days after application (Fig. 6).
- Remind patients to:
- Avoid any food or beverage after each topical application for at least 30 minutes.
- Remove their denture before any use of local therapy (in the case of denture-wearing patients).



Fig. 6: Atrophic candidiasis (a). Partial response of the erythema after 2 weeks of topical antifungal therapy (b). Complete resolution of the lesion after 3 weeks of treatment (c).
Treatment options
- Oral troche is advantageous over suspension due to prolonged contact time with the affected mucosal surface; however, troches need to be prepared by compounding pharmacists and are more costly.
- The commercially available clotrimazole and nystatin topical preparations are usually marketed for other mucocutaneous candidiasis treatments (e.g., for vaginal yeast infections or athlete’s foot); and are intended for external use only. They are safe to apply in or around the mouth/lip, and on dentures.
- Clotrimazole (10 mg oral troches): Dissolve 1 troche in oral cavity 5 times a day.
- Nystatin oral suspension (100 000 U/mL): rinse 5 cc q.i.d. for 2 minutes and expectorate. Caution: commercial preparation might contain cariogenic sweeteners.
- Non-prescription treatments (clotrimazole: 1% cream or nystatin: 100 000 U/g cream or ointment):
- Angular cheilitis patients: Apply a thin layer to the inner and outer corner of mouth q.i.d. after meals.
- Denture-wearing patients: Apply a thin layer to the tissue side of the denture and the infected oral mucosa q.i.d. after meals.
Alternate Systemic Treatments
Periodical liver function tests are suggested for patients with impaired liver function (e.g., due to alcoholism or hepatitis) or for an extended period of usage. Patients with impaired liver function should also be cautioned about possible drug interactions (such as with potent hepatic cytochrome P450 inhibitors).
- Fluconazole tablets (100 mg): 1 tablet q.d. for 2 weeks
- Ketoconazole tablets (200 mg): 1 tablet q.d. for 2 weeks
Advice
- If patient is not responsive to initial antifungal management, refer to oral medicine specialist to investigate a systemic course.
- Not all asthma inhalers contain steroids. If the inhaler enclosure colour is not green or blue, the inhaler contains steroids.
- Other situations for which an oral medicine specialist could provide care include:
- Concurrent candidiasis superimposed on epithelial dysplasia, squamous cell carcinoma, lichen planus
- Oral manifestation of systemic illness (e.g., endocrine dysfunction)
- Monitoring of the safety of systemic antifungal with physician
- Management of contributory factors including xerostomia secondary to drug administration or Sjögren syndrome
- Management of burning mouth syndrome initially presenting as oral candidiasis
THE AUTHOR
Suggested Resources
- Giannini PJ, Shetty KV. Diagnosis and management of oral candidiasis. Otolaryngol Clin North Am. 2011;44(1):231-40.
- Muzyka BC. Oral fungal infections. Dent Clin North Am. 2005;49(1):49-65.

