Abstract
The endocrown is indicated for the endodontic restoration of severely damaged molars. This monolithic, ceramic adhesive restoration requires specific preparation techniques to satisfy criteria that are primarily biomechanical in nature: a cervical margin in the form of a butt joint and a preparation of the pulp chamber that does not extend into the root canals. The remaining tooth substance is thus more robust, resulting in increased longevity. This simple and efficient concept is compatible with the philosophy of biointegrated prostheses. This type of reconstruction, which is still uncommon, should be more widely known and used.
For many practitioners, the use of complete glass ceramic crown restorations for severely damaged and endodontically treated molars remains problematic.1 Proposed in 1999 by Bindl and Mörmann2 as an alternative to the full post-and-core supported crown, the “endocrown” is a one-piece ceramic construction, based on concepts developed by Pissis.3In 2008, Lander and Dietschi4 presented a clinical report on endocrowns, and, in 2009, Magne and Knezevic,5 who were concerned about the choice of reconstruction materials, considered ceramics versus composites for endocrown molar restorations. Various studies suggested extending the concept to maxillary premolars6 and maxillary incisors,7 but these proposals remain controversial.
The main objective is to dispense with metal and achieve an all-ceramic bonded reconstruction that is minimally invasive of root canals, as the use of root canals for anchoring has been cited as an important factor in weakening the tooth.8-11 Thus, the preparation for endocrowns is different from that for conventional complete crowns.12,13
The endocrown is described as a monolithic (one-piece) ceramic bonded construction14-18 characterized by a supra-cervical19 butt joint, retaining maximum enamel to improve adhesion. The endocrown invades the pulpal chamber, but not the root canals. It is milled using computer-aided techniques16,18 or by molding ceramic materials under pressure20,21 (Fig. 1a and b). New generations of ceramics and adhesives may lead to a view of this therapeutic device as an alternative to conventional crown-root anchored restorations.22,23 The specific preparation and bonding result in a particularly favourable reconstruction in terms of biomechanics.5,24,25
NOTE: Click to enlarge images.
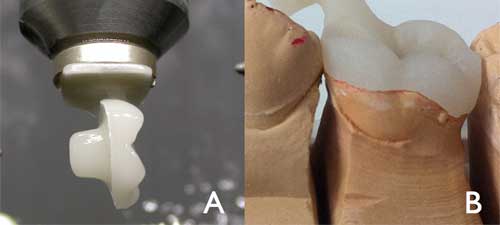 Figure 1: An endocrown machined using computer-aided design and computer-aided manufacture (a). A pressed endocrown, with sprue attached, positioned on a master mold (b).
Figure 1: An endocrown machined using computer-aided design and computer-aided manufacture (a). A pressed endocrown, with sprue attached, positioned on a master mold (b).
The purpose of this paper is to describe the preparation and insertion of endocrowns as well as the materials used to achieve a reliable and durable result.
Methods
Occlusal Preparation
The goal in preparation is to achieve an overall reduction in the height of the occlusal surface of at least 2 mm in the axial direction. This reduction can be achieved by drilling 2-mm-deep grooves as guides (Fig. 2), then using a green diamond wheel bur to reduce the occlusal surface.
The bur is oriented along the major axis of the tooth and held parallel to the occlusal plane (Fig. 3). Its shape allows control of the orientation of the reduction and ensures a flat surface, which determines the position of the cervical margin or “cervical sidewalk.” The cervical margin should be supragingival; however, if clinical factors or esthetics require, the margin can follow the gingival margin. Differences in level between the various parts of the cervical margin must be linked by a slope of no more than 60° to avoid a staircase effect. Enamel walls less than 2 mm thick should be removed.
 Figure 3: Preparation of the cervical margin or “cervical sidewalk” using a wheel bur held parallel to the occlusal plane.
Figure 3: Preparation of the cervical margin or “cervical sidewalk” using a wheel bur held parallel to the occlusal plane.
Axial Preparation
This step primarily involves eliminating undercuts in the access cavity. A cylindrical-conical green diamond bur with a total occlusal convergence of 7° is used to make the coronal pulp chamber and endodontic access cavity continuous (Fig. 4). With the bur orientated along the long axis of the tooth, the preparation is carried out without excessive pressure and without touching the pulpal floor. Removing too much tissue from the pulp chamber walls will reduce their thickness and the width strip of enamel. The depth of the cavity should be at least 3 mm.
 Figure 4: Axial preparation using a cylindro-conical drill to make the coronal pulp chamber continuous with the access cavity.
Figure 4: Axial preparation using a cylindro-conical drill to make the coronal pulp chamber continuous with the access cavity.
Polishing the Cervical Band
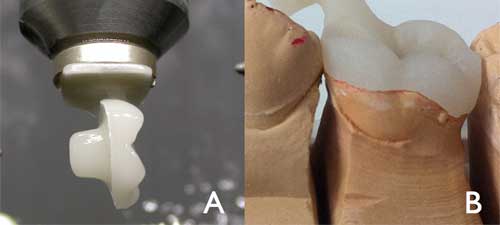
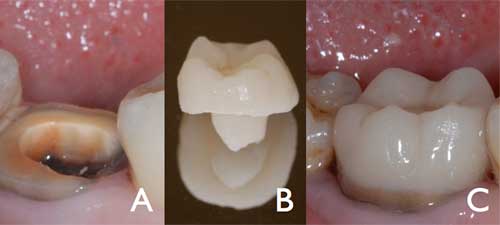
The bur used in this step has the same taper as the one used in axial preparation, but a larger diameter and a finer particle size. It should be guided around the entire surface of the cervical band to remove micro-irregularities and produce a flat, polished surface (Fig. 5). The margin line should appear as a regular line with a sharp edge (Fig. 6a and b).
Preparation of the Cavity Floor
The entrance to the pulpal canal is opened. Gutta percha is removed to a depth not exceeding 2 mm to take advantage of the saddle-like anatomy of the cavity floor. This should be done with a nonabrasive instrument to maintain the integrity of the canals entrance. No drilling of dentin is carried out.
Cleaning the Pulp Chamber
Ultrasound is recommended to clean the pulp chamber and its floor thoroughly. Abrasion is not indicated.
Bonding
Adhesives such as self-adhesive RelyX Unicem (3M, St. Paul, Minn.) or composites such as Multilink (Ivoclar, Schaan, Liechtenstein) are used for bonding the endocrown to the prepared tooth (Fig. 7).
Discussion
Longevity and Effectiveness
In an evaluation of adhesively placed endocrowns after 2 years, Bindl and Mörmann2 concluded that “the overall clinical quality of the endocrowns was very good.” In another 2-year evaluation, Bernhart et al.14 concluded that endocrowns “represent a very promising treatment alternative for endodontically treated molars.” In 2012, Biacchi and Basting26compared the fracture strength of 2 types of full ceramic crowns: indirect conventional crowns retained by glass fibre posts and endocrowns. They concluded that endocrowns were more resistant to compressive forces than conventional crowns. More recently, finite element analysis highlighted the role of endocrowns in stress distribution.27
Indications and Contraindications
The endocrown is suitable for all molars, particularly those with clinically low crowns, calcified root canals or very slender roots. The endocrown is contraindicated if adhesion cannot be assured, if the pulpal chamber is less than 3 mm deep or if the cervical margin is less than 2 mm wide for most of its circumference.
Choice of Materials
Glass-ceramic: Glass-ceramic has the advantages of biocompatibility and biomimicry,15 and its wear coefficient is close to that of the natural tooth.16 In addition, the single interface of a 1-piece restoration enhances cohesion.
Bonding Agent: The bonding material constitutes the critical interface between the restoration and the prepared tooth.21 In addition to its adhesive properties, its modulus of elasticity is important as it must be able to absorb pressure, just as the dentin enamel junction (DEJ) does.22 The interface includes all prepared surfaces. Products that must be photopolymerized require the use of a high-power lamp that must be able to reach light-triggered initiators on the pulpal floor, under layers of ceramic that sometimes exceed 7 mm.
Preparation
The butt joint, or cervical sidewalk, is the base of the restoration — with a band of peripheral enamel that optimizes bonding.19 Unlike chamfer or shoulder preparation techniques, crimping is prohibited. The goal is to achieve a wide, even, stable surface that resists the compressive stresses that are most common on molars.8 The prepared surface is parallel to the occlusal plane to ensure stress resistance along the major axis of the tooth.
The pulpal chamber cavity ensures retention and stability. Its shape — trapezoidal in mandibular molars and triangular in maxillary molars — enhances the restoration’s stability.
There is no need for additional preparation. The saddle form of the pulpal floor enhances stability. This anatomy, along with the adhesive qualities of the bonding material, makes it unnecessary to attempt further use of post involving root canals. Actually the root canals do not require any specific shape; therefore they are not weakened by the drilling11 and they will not be subject to the stresses associated with the use of post.8,9 The compressive stresses are reduced, being distributed over the cervical butt joint and the walls of the pulp chamber.
Conclusion
The preparation for endocrowns is rational and simple and can be performed quickly. Root canals are not involved in the process, and the procedure is less traumatic than alternatives. The supragingival position of the cervical margin preserves the marginal periodontium, facilitates impression taking and maintains the solid substance of the remaining tooth. The all-ceramic monolithic-type construction, made by pressure molding or machining, endows the endocrown with mechanical strength. From a biomechanical standpoint, the restoration allows adaptation to strains at the bonded joint. These forces are distributed over the cervical butt joint (compression) and axial walls (shear force), thus moderating the load on the pulpal floor. The endocrown fits perfectly with the concept of biointegration and belongs among the restorative options for posterior endodontically treated and badly damaged molars.
THE AUTHORS
References
- Zahran M, El-Mowafy O, Tam L, Watson PA, Finer Y. Fracture strength and fatigue resistance of all-ceramic molar crowns manufactured with CAD/CAM technology. J Prosthodont. 2008; 17(5): 370-7.
- Bindl A, Mörmann WH. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years — preliminary results. J Adhes Dent. 1999;1(3):255-65.
- Pissis P. Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract Periodontics Aesthet Dent. 1995;7(5): 83-94.
- Lander E, Dietschi D. Endocrowns: a clinical report Quintessence Int. 2008;39(2):99-106.
- Magne P, Knezevic A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence Int. 2009;40(2):125-33.
- Lin CL, Chang YH, Chang CY, Pai CA, Huang SF. Finite element and Weibull analyses to estimate failure risks in the ceramic endocrown and classical crown for endodontically treated maxillary premolar. Eur J Oral Sci. 2010;118(1): 87-93.
- Zarone F, Sorrentino R, Apicella D, Valentino B, Ferrari M, Aversa R et al. Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endocrowns compared to a natural tooth: a 3D static linear finite elements analysis. Dent Mater. 2006;22(11):1035-44. Epub 2006 Jan 10.
- Zogheib LV, Saavedra Gde S, Cardoso PE, Valera MC, Araújo MA. Resistance to compression of weakened roots subjected to different root reconstruction protocols. J Appl Oral Sci. 2011;19(6):648-54.
- Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont. 2001;14(4):355-63.
- Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent. 2005;93(2):164-70.
- Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont. 2001; 14(4):355-63.
- Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001 Apr;85(4):363-76.
- Schillingburg HT, Hobo S, Whitsett LD, Jacobi R, Brackett SE. Fundamentals of fixed prosthodontics. Chicago: Quintessence; 1997.
- Bernhart J, Bräuning A, Altenburger MJ, Wrbas KT. Cerec3D endocrowns — two-year clinical examination of CAD/CAM crowns for restoring endodontically treated molars. Int J Comput Dent. 2010;13(2):141-54.
- Höland W, Schweiger M, Watzke R, Peschke A, Kappert H. Ceramics as biomaterials for dental restoration. Expert Rev Med Devices. 2008;5(6):729-45.
- Qin F, Zheng S, Luo Z, Li Y, Guo L, Zhao Y, Fu Q. Evaluation of machinability and flexural strength of a novel dental machinable glass-ceramic. J Dent. 2009;37(10):776-80. Epub 2009 Jun 16.
- Messer RL, Lockwood PE, Wataha JC, Lewis JB, Norris S, Bouillaguet S. In vitro cytotoxicity of traditional versus contemporary dental ceramics. J Prosthet Dent. 2003;90(5):452-8.
- Vitablocs MarkII for Cerec. Materials sciences and clinical studies. Brea, Cal.: Vident; 2009. [accessed 2013 Aug 27] Available: http://vident.com/wp-content/uploads/2009/01/cerecmarkii.pdf.
- Donovan TE, Chee WW. Cervical margin design with contemporary esthetic restorations. Dent Clin North Am. 2004;48(2):vi, 417-31.
- Mrazek WR. Laboratory procedures for fabricating pressable all-ceramic restorations. J Dent Technol. 1997;14(4):10-6.
- Mrazek WR. Laboratory procedures for fabricating pressable all-ceramic restorations. J Dent Technol. 1997;14(3):21-31.
- Bindl A, Richter B, Mörmann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int J Prosthodont. 2005;18:219-24.
- Guarda GB, Gonçalves LS, Correr AB, Moraes RR, Sinhoreti MA, Correr-Sobrinho L. Luting glass ceramic restorations using a self-adhesive resin cement under different dentin conditions. J Appl Oral Sci. 2010;18(3):244-8.
- Slangen P, Corn S, Fages M, Cuisinier FJ. Prosthodontic crown mechanical integrity study using Speckle Interferometrie In: Osten W, Kujawinska M, editors. Fringe 2009: 6th International Workshop on Advanced Optical Metrology. Berlin Heidelberg: Springer; 2009. pp. 734-8.
- Zaslansky P, Friesem AA, Weiner S. Structure and mechanical properties of the soft zone separating bulk dentin and enamel in crowns of human teeth: insight into tooth function. .J Struct Biol. 2006;153(2):188-99. Epub 2005 Dec 9.
- Biacchi GR, Basting RT. Comparison of fracture strength of endocrowns and glass fiber post-retajned conventinal crowns. Oper Dent. 2012;37(2):130-6.
- Hasan I, Frentzen M, Utz KH, Hoyer D, Langenbach A, Bourauel C. Finite element analysis of adhesive endo-crowns of molars at different height level of bucally applied load. J Dent Biomech. 2012; 3:1758736012455421.
| Gallery of all Figures in article. | |||
 |
 |
 |
 |
 |
 |
 |
|


