Case Report
A 41-year-old man was referred to us complaining of jaw dislocation, joint sounds, limitation of opening and pain on chewing. He reported progressive facial asymmetry that had developed slowly over 18 months and was clearly visible. Physical examination revealed mandibular prognathism and a 13-mm deviation of the mandibular midline to the left. The patient’s maximum jaw opening was 36 mm. A bilateral clicking sound could be heard during mandibular movements. No pain on palpation of the temporomandibular joints (TMJs) was present. Masseter muscles were mildly painful to palpation. He had a unilateral posterior cross-bite on the left side, 4-mm negative horizontal overjet and a class III molar occlusal relationship (Fig. 1).
A panoramic radiograph showed a radiopaque mass attached to the right condyle. The density of the lesion was similar to that of adjacent bone (Fig. 2). The mass had a beak-like appearance and projected anterior to the right articular eminence. Coronal, axial and cone-beam computerized tomography images revealed a lesion with cartilaginous features developing on the condylar head (Fig. 3). The lesion had developed medially and superiorly to pterygoid muscle fibres, causing erosion of the base of the cranial cortex superiorly. No translation was possible with the right condyle while the left condyle showed a 13.20-mm translation.
NOTE: Click to enlarge images.
 Figure 1: Frontal view of the occlusion at presentation showing severe left posterior cross-bite, 4-mm negative horizontal overjet and severe deviation of the midline to the left.
Figure 1: Frontal view of the occlusion at presentation showing severe left posterior cross-bite, 4-mm negative horizontal overjet and severe deviation of the midline to the left.
Before surgery, study models and occlusal records were taken. Minor occlusal adjustment was performed, but no orthodontic tooth movement was considered necessary to ensure postoperative occlusal stability. The periodontal condition and the rapid evolution of the disease excluded decompensation orthodontic treatment.
Under general anesthesia, pre-auricular and submandibular approaches were used to access the right ramus. An extraoral vertical ramus osteotomy was performed and the proximal segment containing the condyle and the lesion was removed (Fig. 4). The tooth-bearing segment of the mandible was placed in adequate occlusion correcting the midline shift, and intermaxillary fixation was applied. On the table, the lesion was excised from the condylar head along with a 2-mm margin of normal tissue. After reshaping of the condylar head, the condylar segment was repositioned back into the condylar fossa and stabilized with rigid fixation. At this point, the intermaxillary fixation was removed and midline alignment was confirmed.
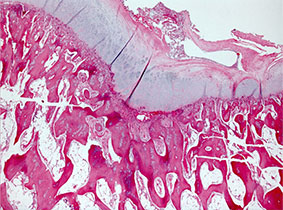
The excised tumour measured 3 cm × 2 cm × 1 cm. Microscopic examination of the decalcified tissue revealed a layer of hyaline cartilage containing benign chondrocytes in their lacunae. This cartilage formed a cap overlying normal-appearing trabeculae of cancellous bone (Fig. 5). The cartilaginous cap was covered by a layer of fibrous connective tissue (perichondrium). The osteochondral junction resembled growth plates with chondrocytes arranged perpendicular to the surface.
What is the diagnosis?
Microscopic features of the tumour were consistent with a diagnosis of osteochondroma.
Osteochondroma, also termed osteocartilaginous exostosis, is a sessile or pedunculated benign chondrogenic tumour that arises in any bone in which endochondral ossification occurs. It is the most common benign bone tumour of the axial skeleton, but is rare in the craniofacial complex, primarily because of the intramembranous development of these bones. Reported regions of occurrence in the craniofacial skeleton include the skull base, maxillary sinus, zygomatic arch and mandible. Mandibular osteochondromas have been reported to occur in the coronoid process, condyle, ramus, body, angle and symphysis regions.1-4 The coronoid and condylar processes have been considered to be the most common sites of occurrence of osteochondroma of the facial skeleton.5-12 Typical clinical features of condylar osteochondroma include progressive facial asymmetry, chin deviation, and cross-bite to the contralateral side, changes in condylar morphology and malocclusion with open bite on the affected side.1,5,8,13
Differential diagnosis should include condylar hyperplasia, hemifacial hyperplasia (hypertrophy) as well as benign tumours of bony or cartilaginous origin involving the mandibular condyle.
Compared with osteochondroma, condylar hyperplasia is usually diagnosed earlier in life, most commonly in adolescents and young adults. During active growth, proliferation of the condylar cartilage is noted and the histology could be similar to osteochondroma. However, radiographic features, such as irregular enlargement of the condylar head with preservation of its anatomy, elongation of the condylar neck and the absence of a protruding mass, favour a diagnosis of condylar hyperplasia.14
Asymmetry secondary to hemifacial hyperplasia is noted at birth and continues during development to become more accentuated at puberty. The soft tissues, bone and teeth on the affected side are enlarged,15 a feature that can distinguish this from condylar hyperplasia. In contrast, facial asymmetry secondary to osteochondroma is slowly progressive, of recent onset and does not cause soft tissue changes. Radiographic features can also help distinguish between a neoplastic process such osteochondroma and a developmental process such as hemifacial hyperplasia.
The most common benign tumours of osseous and cartilaginous origin involving the condyle are osteomas, chondromas and osteochondromas. Osteomas are composed of mature compact or cancellous bone, which helps to differentiate them radiographically and histopathologically from osteochondromas. They occur in the craniofacial skeleton and are rarely diagnosed in other bones. The most common gnathic locations are the body of the mandible and the condyle. When the condyle is involved, the tumour is often located at the anteromedial region at the level of insertion of the lateral pterygoid muscle. This is also the location of osteochondromas of the TMJ. Osteomas involving the mandibular condyle may also cause a slowly progressive shift in the patient’s occlusion, with deviation of the midline toward the unaffected side. Other reported complaints include facial swelling, pain and limited opening.
Chondromas are benign tumours composed of mature cartilage. They are much more common in the small bones of the hands and feet than in the jaw bones where chondrogenic tumours are rare. Malignancy should always be suspected in gnathic chondromas and numerous histologic fields of the lesion must be carefully examined to confirm its benign nature.15 Jaw chondromas present as painless, slowly growing tumours. However, tooth mobility and root resorption are noted with some lesions. Condylar chondromas are rare and few cases have been reported in the literature. They can produce the same symptoms as osteochondromas, including limitation of jaw movements, deviation on opening and occlusal changes. Histopathologic examination allows distinction between osteochondroma and chondroma.
Osteochondromas are characterized histologically by a cartilaginous cap covering an osseous growth.14 The cap has an appearance similar to a growth plate with chondrocytes arranged in parallel rows perpendicular to the surface. A layer of fibrous connective tissue (perichondrium) covers the surface. The deeper part of the cap (osteochondral junction) shows endochondral ossification with cancellous bone production that blends with underlying normal bone.
Treatment
Condylectomy is the conventional treatment for osteochondroma affecting the mandibular condyle14 with no reported recurrences of condylar lesions after surgical treatment.1,6,14 An overall recurrence rate of about 2% is reported in other sites.1 To take advantage of the exophytic and non-invasive nature of the disease, Wolford et al.6 suggested a conservative condylectomy that consists of resecting the tumour with preservation of some or all of the condylar head. This approach was used in the case presented here. The tumour was resected under direct vision on the table allowing the surgeon to ensure complete resection and, therefore, a low recurrence rate. After reshaping of the condylar stump, the segment was repositioned and fixed in place while the malocclusion was corrected.
The follow-up shows that the initial cross-bite and the malocclusion, corrected at the time of surgery, were stable 1 year post-operatively (Fig. 6). Similarly, the inter-incisal opening was 37 mm without evidence of loss in the range of motion. An orthopantomogram did not show any evidence of recurrence at the time of this follow-up. We therefore recommend this approach in cases of condylar OC, when judged surgically feasible. Reporting such cases will allow oral and maxillofacial surgeons to be more comfortable to offer this treatment modality to patients affected by this disease.
 Figure 6: Frontal view of the occlusion 6 months after surgery showing normal overjet, overbite and molar relationship. A minor deviation (1 mm) of the mandibular midline to the left side remained.
Figure 6: Frontal view of the occlusion 6 months after surgery showing normal overjet, overbite and molar relationship. A minor deviation (1 mm) of the mandibular midline to the left side remained.
THE AUTHORS
| Gallery of all Figures in article | |||||
 |
 |
 |
 |
 |
 |
References
- Iizuka T, Schroth G, Laeng RH, Lädrach K. Osteochondroma of the mandibular condyle: report of a case. J Oral Maxillofac Surg. 1996;54(4):495-501.
- Tanaka E, Iida S, Tsuji H, Kogo M, Morita M. Solitary osteochondroma of the mandibular symphysis. Int J Oral Maxillofac Surg. 2004;33(6):625-6.
- Karras SC, Wolford LM, Cottrell DA. Concurrent osteochondroma of the mandibular condyle and ipsilateral cranial base resulting in the temporomandibular joint ankylosis: report of a case and review of the literature. J Oral Maxillofac Surg. 1996;54(5):640-6.
- Koga K, Toyama M, Kurita K. Osteochondroma of the mandibular angle: report of a case. J Oral Maxillofac Surg. 1996;54(4):510-3.
- Koole R, Steenks MH, Witkamp TD, Slootweg PJ, Shaefer J. Osteochondroma of the mandibular condyle. A case report. Int J Oral Maxillofac Surg. 1996;25(3):203-5.
- Wolford LM, Mehra P, Franco P. Use of conservative condylectomy for treatment of osteochondroma of the mandibular condyle. J Oral Maxillofac Surg. 2002;60(3):262-8.
- Herbosa EG, Rotskoff KS. Condylar osteochondroma manifesting as Class III skeletal dysplasia: diagnosis and surgical approach. Am J Orthod Dentofacial Orthop. 1991;100(5):472-9.
- Ward BB, Pires CA, Feinberg SE. Osteochondromas of the mandible: case reports and rationale for treatment. J Oral Maxillfac Surg. 2005;63(7):1039-44.
- Muñoz M, Goizueta C, Gil-Díez JL, Díaz FJ. Osteocartilaginous exostosis of the mandibular condyle misdiagnosed as temporomandibular joint dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(5):494-5.
- Aydin MA, Küçükçelebi A, Sayilkan S, Celebioğlu S. Osteochondroma of the mandibular condyle: report of 2 cases treated with conservative surgery. J Oral Maxillofac Surg. 2001;59(9):1082-9.
- Henry CH, Granite EL, Rafetto LK. Osteochondroma of the mandibular condyle: report of a case and review of the literature. J Oral Maxillofac Surg. 1992;50(10):1102-8.
- Marks RB, Carlton DM Jr, Carr RF. Osteochondroma of the mandibular condyle. Report of a case with 10-year follow-up. Oral Surg Oral Med Oral Pathol. 1984;58(1):30-2.
- Stevao EL. Osteochondroma of the mandibular condyle: conservative reconstruction with condylectomy. J Oral Maxillofac Surg. 2003;61:65.
- Roychoudhury A, Bhatt K, Yadav R, Bhutia O, Roychoudhury S. Review of osteochondroma of mandibular condyle and report of a case series. J Oral Maxillofac Surg. 2011;69(11):2815-23. Epub 2011 Mar 2.
- Neville B, Damm D, Allen C, Bouquot J. Oral and Maxillofacial Pathology, 3rd ed. Toronto: W.B. Saunders Company. 2008