Peri-implantitis
Infectious disease that causes an inflammatory process in the soft and hard tissues surrounding an osseointegrated implant, leading to the loss of supporting bone.
Presentation
Population
Patients with implants
Risk Factors
- Tobacco use
- Poorly controlled systemic conditions (e.g., diabetes mellitus, osteoporosis, post-irradiated jaws)
- History of periodontitis and noncompliance to treatment
- Poor oral hygiene
- Parafunctional habits (e.g., bruxism)
- Iatrogenic factors (e.g., lack of primary stability and premature loading during the healing period)
Signs
- Progressive increase in probing depth
- Suppurations and exudation from peri-implant space
- Bleeding on probing
- Clinical appearance of inflamed tissue (bleeding, swelling, colour change, suppuration, and plaque/calculus accumulation)
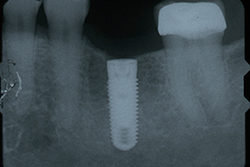
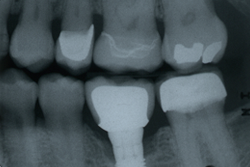
- Progressive loss of supporting bone on follow-up radiographs (Figs. 1 and 2): loss of supporting bone beyond 0.2 mm annually, after the expected physiologic remodelling.
NOTE: Click to enlarge images.
Symptoms
- Not always symptomatic
- Pain severity: typically none
- May have dull aches, tenderness on brushing or palpation
- Bad taste: potentially noticeable if there are purulent exudates
- Increasing mobility (in cases of a failed implant)
- Lymphadenopathy
Investigation
- Verify if iatrogenic factors are involved such as faulty restoration, impacted foreign material (residual cement), loose components, etc.
- Assess if inadequate biomechanical forces are applied by evaluating the occlusion for the presence of:
- Parafunction
- Occlusal overload
- Mobility of the restorative component (remove crown to assess whether implant is mobile), fractured restorative component, fractured implant
- Look for active periodontitis in other sites.
- Assess the potential of other bone pathologies.
- Perform an exploratory surgery.
Diagnosis
Based on the clinical and radiographic evaluation, a diagnosis of peri-implantitis is determined.
Differential Diagnosis
Peri-implant mucositis
Treatment
The long-term goals are to stop the progression of the disease and maintain the implant site. Depending on the etiology of the problem, a specific treatment is selected. Appropriate management of peri-implantitis often requires referral to a periodontist.
Etiology: Bacterial Infection
- Control the acute bacterial infection and reduce the inflammation in the tissues through:
- Mechanical debridement
- Localized and/or systemic antimicrobial therapy
- Improved patient compliance with oral hygiene until a healthy peri-implant site is established
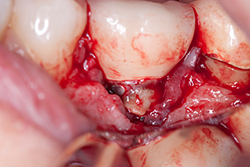
- At the re-evaluation, if the patient does not have a satisfactory response to the nonsurgical therapy, surgery should be considered. Assess the presence of retained cement and its subsequent removal (Figs. 3 and 4). It is important to assess for possible cement entrapment, as new data shows an increasing number of failures from this etiology.
- Detoxify the implant surface by using mechanical devices (e.g., high pressure air powder abrasive, laser decontamination) and/or by applying chemotherapeutic agents (e.g., supersaturated citric acid or tetracycline applied with cotton pellets or a brush).
- Perform flap management with either (or both) resective and regenerative approaches, depending on the morphology and size of the bone destruction.
- Systemic antibiotics are suggested postoperatively.
Etiology: Biomechanical Forces
- Perform:
- an analysis of the fit of the prosthesis
- a verification of the number and position of the implants
- an occlusal evaluation
Prostheses design changes, replacing defective restorative components, and correcting occlusal overload (through improvement of implant number and position, occlusal equilibration, and occlusal splint for patients with parafunction) can arrest the progression of peri-implant tissue breakdown.
- Perform the surgical procedure, if necessary.
- Detoxify the implant surface by using mechanical devices (e.g., high pressure air powder abrasive, laser decontamination) and/or by applying chemotherapeutic agents (e.g., supersaturated citric acid or tetracycline applied with cotton pellets or a brush).
- Perform flap management with either or both resective and regenerative approaches, depending on the morphology and size of the bone destruction.
- Systemic antibiotics are suggested postoperatively.
Etiologies Acting as Co-Factors
Other etiologic factors may act as co-factors in the development of peri-implantitis. Nonetheless, treatment still consists of removing the bacterial infection or correcting the biomechanical forces.
Possible Co-Factors
- Anatomical limitations: inadequate amount of bone in recipient site at the time of the implant placement
- Surgical trauma: overheating of bone during implant placement
- Compromised host response
Addressing Potential Risk Factors
- Treatment of active periodontal disease and improvement of oral hygiene
- Counseling the patient on tobacco cessation
Notes
- There is no consensus regarding the best regenerative material and no long-term data regarding success of regenerative treatment.
- It is important for patients to understand that regenerations are neither predictable nor reliable on an integrated and restored implant. Patients must be involved in the decision to save or replace the implant.
- Many techniques for implant surface detoxification have been used but there is not yet a defined standard protocol.
Treatment of Failed Implants
In the presence of extensive bone loss or implant mobility, the implant may be removed and alternative options to replace the missing tooth should be discussed (replacement of failed implant, fixed partial denture, removable partial denture, etc.).
THE AUTHORS
Suggested Resources
- Iacono VJ; Committee on Research, Science and Therapy, the American Academy of Periodontology. Dental implants in periodontal therapy. J Periodontol. 2000;71(12):1934-42.
- Lindhe J, Meyle J; Goup D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(8 Suppl):282-5.
- Heitz-Mayfield L, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. Int J Oral Maxillofac Implants. 2009;24 Suppl:39-68.
- Newman MG,Takei H, Klokkevold PR, Carranza FA. Carranza’s Clinical Periodontology: Expert Consult. 11th ed. St. Louis, Missouri: Elsevier, 2011.
- Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, Missouri: Elsevier, 2008.
- Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science? J Periodontol. 2002;73(3):322-33.
- Jovanovic SA. The management of peri-implant breakdown around functioning osseointegrated dental implants. J Periodontol. 1993;64(11 Suppl):1176-83.