Abstract
Pre-eruptive intracoronal resorption (PEIR) appears as a radiolucent lesion in the coronal dentine, adjacent to the dentin–enamel junction of unerupted teeth. Although PEIR resembles dental caries on radiographs, there is little evidence to support that hypothesis. The prevalence of this lesion varies from 1.55% to 6% depending on the type and quality of the radiographic exposure and age of patients. This case study describes a post-eruptive diagnosis of intracoronal resorption with unusually extensive destruction of dentine involving pulp. It emphasizes the importance of early diagnosis of this resorptive process through radiographs to minimize its potentially destructive capacity.
Dental practitioners may occasionally encounter radiographs of unerupted teeth showing unusual intracoronal radiolucencies in dentin.1 Clinical symptoms are usually minimal or absent, and, typically, such teeth present as incidental findings on routine dental radiographs of unerupted teeth.2–5 Characteristically, the outer surface of the occlusal aspect of the crown remains intact, but a large lesion may be present in the coronal dentin adjacent to the dentin–enamel junction.6-13 The radiographic appearance of the radiolucency is similar to that of dental caries, hence the terms "pre-eruptive caries," "occult caries" and "hidden caries" used in earlier literature.3,11,14 However, there is little histopathologic or microbiologic evidence to support the hypothesis that these lesions are carious in nature when the tooth is unerupted2 and, therefore, more recently the term "pre-eruptive intracoronal resorption" (PEIR) has been used to better denote the etiology and nature of the lesions.2,6,8,10,12
The prevalence of PEIR has been reported to be between 1.55% and 6%1,2,14,15 or greater when third molars are included.1 No association with sex, race, medical status, systemic disease or fluoride supplementation has been found.1,2,14,15 Usually, a single tooth is affected and almost half of these lesions extend to no more than two-thirds of the thickness of the dentin.1,3,4,15
The pathogenesis of PEIR is unclear, as the developing tooth is encased in its crypt and is not likely to have been infected with cariogenic microorganisms.14 Histologic examination of the lesions' soft tissue has revealed resorptive cells (osteoclasts and macrophages) and scalloped lesion borders.1,5,16–18 Thus, it has been hypothesized that local factors, such as damage to the reduced enamel epithelium of unerupted teeth, may allow invasion of cells from the surrounding bony tissue to the surface of the developing tooth.1,2
Case reports have shown significant variation in the clinical course of PEIR radiolucencies. However, progress of the lesion is usually slow before the tooth erupts.6,12,16,19 Most of the defects that have been observed at this stage remain adjacent to the dentin–enamel junction, rarely extending into the pulp.1,6,15,20 However, once the affected tooth emerged into to the oral cavity, conditions become appropriate for rapid development of caries.5,7
Most lesions remain undetected because of the lack of early clinical symptoms and the problems involved in achieving an optimum view in bite-wing radiographs of the mixed dentition. The purpose of this case study is to describe successful management of late clinical presentation of a mandibular premolar with PEIR and to elaborate on strategies for the prevention of similar clinical presentations of what is a relatively common, but often undiagnosed, condition.
Case Report
A 12-year-old patient reported to a pediatric dental clinic at a university teaching hospital. He had previously attended the same clinic at 8 years of age, but had failed to attend any appointments since then. His chief complaint was spontaneous, throbbing pain with associated swelling in the left mandibular area. The child had been unable to chew on the affected side for 12 h. There was no history of trauma, and medical history revealed good general health.
During extra-oral examination, a diffuse soft and mobile swelling was palpated on the left lateral surface of the mandible, extending inferiorly down to the lower border of the mandible (Fig. 1). Submandibular lymph glands on both sides were palpable and tender.
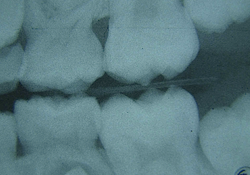
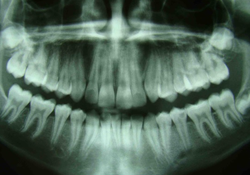
Intra-oral examination of the soft tissues revealed a slight colour change in the patient's left mandibular area, which was particularly sensitive to palpation (Fig. 2). The hard tissues appeared normal and the patient was caries free. Further examination of the patient's left mandibular quadrant revealed that the second premolar (tooth 35) showed a small degree of rotation, grade II+ mobility and pain on percussion, which indicated likely inflammation in the periapical tissues. Bite-wing radiographs were available from the patient's previous visit 4 years earlier (Fig. 3) and further panoramic (Fig. 4) and periapical radiographs were taken to support the clinical diagnosis and treatment decisions.
NOTE: Click to enlarge images.
Radiographic examination revealed a large radiolucent area under the occlusal dentin–enamel junction of tooth 35 and widening of the lamina dura. A cold test was negative, and the tooth was determined to have an acute periapical abscess. A decision was made to start root canal treatment.
To relieve pressure, local anesthesia (Lidocaine HCI 2% with epinephrine 1:100 000) was administered to establish drainage from the coronal portion of the tooth by opening the pulp chamber. Gaining initial access was particularly difficult because of exquisite tenderness of the tooth. Once access and initial drainage had been achieved, a rubber dam was placed and the pulp chamber was thoroughly irrigated with 5% sodium hypochlorite (NaOCl) to remove as much superficial organic and inorganic debris as possible. The working length was estimated to be 1 mm short of the radiographic apex before preparation of the canal. During preparation, the canal was irrigated copiously with 5% NaOCl and normal saline. The pulp chamber and root canal were dried, and a calcium hydroxide dressing was placed in the canal. A dry sterile cotton wool pellet was placed in the pulp chamber with a temporary filling (Cavit, 3M ESPE, Neuss, Germany) to seal the access cavity.
Amoxicillin was prescribed (500-mg tablet every 8 h for 7 days) as part of the emergency treatment, and the patient was scheduled for a further appointment 7 days later. When the patient returned, he was completely free of symptoms. The calcium hydroxide dressing was removed gently using 5% NaOCl and normal saline. Cleaning and shaping was done using a crown down technique with ProTaper files (Dentsply, Maillefer, Ballaigues, Switzerland) with copious irrigation with 5% NaOCl solution. Obturation was performed with root canal sealer (AH plus, Dentsply De Trey GmbH, Konstanz, Germany) and warm gutta-percha, and post-obturation radiographs were taken (Fig. 5). After an uneventful waiting period of 1 week, the access cavity was reopened and final restoration was completed with hybrid resin composite (Filtek Z250 Universal, 3M ESPE, St. Paul, Minn., USA) and bonded with an etch-and-rinse adhesive (Adper Single Bond Plus, 3M ESPE).
 Figure 5: Immediate postoperative radiograph with rubber dam clamp revealing a good seal of the canal.
Figure 5: Immediate postoperative radiograph with rubber dam clamp revealing a good seal of the canal.
Discussion
This case of PEIR was not diagnosed at the pre-eruptive stage as radiographs of the area were not obtained. However, the presentation of an intact outer enamel surface along with a large radiolucent area in the dentin suggested that PEIR was the most likely definitive diagnosis.7,15,21
The patient was otherwise caries free, making a diagnosis of caries unlikely; no radiolucent areas or signs of early caries lesions were seen in any teeth other than tooth 35. Furthermore, symptoms had started suddenly, without being preceded by the typical symptoms of pulpitis, such as sensitivity to heat and cold, and the patient's history and clinical and radiographic examinations showed no signs of trauma. Enamel hypoplasia was discounted as a possible cause of the lesion, as it was considered to be unlikely in the absence of any signs of developmental defects in the remaining dentition. Turner's hypoplasia might also be considered, but the patient's earlier bite-wing radiographs did not show any signs of infection in his primary molars.
The prognosis for teeth affected by PEIR will depend on the size of the lesion at the time of discovery.20 Therefore, management and limitation of damage depend on early diagnosis through radiographs. Radiographs of children's teeth are usually taken to detect caries and orthodontic problems.15 However, because of the relatively high prevalence of PEIR,15 it might be prudent to suggest that all unerupted teeth discovered on bite-wing and other intra- and extra-oral radiographs be routinely scrutinized for PEIR.1,2 Where an intracoronal radiolucency is detected in an unerupted developing tooth, the tooth can be re-examined with a more detailed radiograph21 to confirm the diagnosis and the tooth can be treated accordingly.
If a relatively small lesion is discovered in a tooth, it may be monitored carefully until after tooth eruption when the cavity may be routinely restored.8 Holan et al.12 described pulp reaction in PEIR before eruption and, therefore, authors have recommended that, when lesions are large and appear to be encroaching on the pulp, care should be taken to expose the tooth surgically and restore it to protect pulp vitality and facilitate normal root development.8,10,15,21
The present case demonstrates a post-eruptive diagnosis of intracoronal resorption with unusually substantial destruction of dentin involving pulp. Although the patient attended the clinic as a new patient 4 years earlier when 2 bite-wing and 2 occlusal radiographs were taken, because of the small size of the bite-wing films, only the cusp tips of premolars were seen and the intracoronal radiolucency was not diagnosed in tooth 35. At the time, the parents refused to allow a routine panoramic radiograph to monitor growth and development, as they were hesitant to agree to expose their child to further radiation. A decision had been made to take a panoramic radiograph on the next recall appointment (6 months later); however, the patient had not attended that or any later recall appointments.
Conclusion
This case demonstrates that enlarged defects caused by PEIR can easily threaten the pulp tissue within a short time during tooth eruption and that PEIR may be an important cause of unusual pulpal abscesses in children.
As unerupted permanent teeth may not always appear in optimum view in bite-wing radiographs of the mixed dentition, a panoramic radiograph should be considered, based on the recommendations of the American Dental Association and the United States Food & Drug Administration. Had an earlier diagnosis been possible, the need for root canal treatment would have been avoided in an otherwise caries-free patient.
As recurrence of resorption after restoration of the cavity has not been reported,7 early diagnosis and treatment of PEIR will prevent the distress of pain, infection and extensive treatment after tooth eruption.
THE AUTHOR
| Gallery of all Figures in article | ||||
 |
 |
 |
 |
 |
References
- Seow WK, Lu PC, McAllan LH. Prevalence of pre-eruptive intracoronal dentin defects from panoramic radiographs.Pediatr Dent. 1999;21(6):332-9.
- Seow WK, Wan A, McAllan LH. The prevalence of pre-eruptive dentin radiolucencies in the permanent dentition. Pediatr Dent. 1999;21(1):26-33.
- Brooks JK. An unusual case of idiopathic internal root resorption beginning in an unerupted permanent tooth. J Endod. 1986;12(7):309-10.
- Rutar JE. Paediatric dentistry: coronal radiolucency. Case reports. Aust Dent J. 1997;42(4):221-4.
- McNamara CM, Foley T, O'Sullivan VR, Crowley N, McConnel RJ. External resorption presenting as an intracoronal radiolucent lesion in a pre-eruptive tooth. Oral Dis. 1997;3(3):199-201.
- Seow WK. Multiple pre-eruptive intracoronal radiolucent lesions in the permanent dentition: case report. Pediatr Dent. 1998;20(3):195-8.
- Seow WK. Diagnosis and management of unusual dental abscesses in children. Aust Dent J. 2003;48(3):156-68.
- Davidovich EB, Kreiner B, Peretz B. Treatment of severe pre-eruptive intracoronal resorption of a permanent second molar. Pediatr Dent. 2005;27(1):74-7.
- Nik NN, Abul Rahman R. Pre-eruptive intracoronal dentin defects of permanent teeth. J Clin Pediatr Dent. 2003;27(4):371-5.
- Seow WK, Hackley D. Pre-eruptive resorption of dentin in the primary and permanent dentitions: case reports and literature review. Pediatr Dent. 1996;18(1):67-71.
- Giunta JL, Kaplan MA. "Caries-like" dentin radiolucency of unerupted permanent tooth from developmental defects. J Pedod. 1981;5(3): 249-55.
- Holan G, Eidelman E, Mass E. Pre-eruptive coronal resorption of permanent teeth: report of three cases and their treatments. Pediatr Dent. 1994;16(5):373-7.
- Rankow H, Croll TP, Miller AS. Preeruptive idiopathic coronal resorption of permanent teeth in children. J Endod. 1986;12(1):36-9.
- Seow WK. Pre-eruptive intracoronal resorption as an entity of occult caries. Pediatr Dent. 2000;22(5):370-6.
- Özden B, Acikgoz A. Prevalence and characteristics of intracoronal resorption in unerupted teeth in the permanent dentition: a retrospective study. Oral Radiol. 2009;25(1):6-13.
- Klambani M, Lussi A, Ruf S. Radiolucent lesion of an unerupted mandibular molar. Am J Orthod Dentofacial Orthop. 2005;127(1):67-71.
- O'Neal KM, Gound TG, Cohen DM. Preeruptive idiopathic coronal resorption: a case report. J Endod. 1997;23(1):58-9.
- Taylor NG, Gravely JF, Hume WJ. Resorption of the crown of an unerupted permanent molar. Int J Paediatr Dent. 1991;1(2):89-92.
- Hata H, Abe M, Mayanagi H. Multiple lesions of intracoronal resorption of permanent teeth in the developing dentition: a case report. Pediatr Dent. 2007;29(5):420-5.
- Moskovitz M, Holan G. Pre-eruptive intracoronal radiolucent defect: a case of a nonprogressive lesion. J Dent Child (Chic). 2004;71(2):175-8.
- Counihan KP, O'Connell AC. Case report: pre-eruptive intra-coronal radiolucencies revisited. Eur Arch Paediatr Dent. 2012;13(4):221-6.