Abstract
Objective: To estimate the strength of the associations among income, dental insurance coverage and need for dental care (both urgent and nonurgent) in Canada.
Methods: Multinomial logistic models were fit to data from the 2009 Canadian Health Measures Survey to test unadjusted associations among household income, dental insurance coverage and the need for urgent and nonurgent dental care. Adjusted associations, controlling for socio-demographic variables (age, sex, immigration status, education and province of residence) and oral health habits (brushing, flossing and visits to the dentist) were also evaluated.
Results: In the unadjusted model, need for treatment was lower among people with dental insurance than among those without insurance coverage (for urgent treatment: odds ratio [OR] 0.76, 95% confidence interval [CI] 0.66–0.89; for nonurgent treatment: OR 0.59, 95% CI 0.50–0.70). In addition, there was an income gradient, whereby people with higher income had less need for dental treatment (for urgent treatment: OR 0.99, 95% CI 0.99–1.00; for nonurgent treatment: OR 0.99, 95% CI 0.98–0.99). Controlling for socio-demographic and oral health variables decreased the magnitude of the association between dental insurance coverage and need for treatment (for urgent treatment: OR 0.80, 95% CI 0.68–0.95; for nonurgent treatment: OR 0.76, 95% CI 0.63–0.92). An interaction term between dental coverage and income was significant in relation to the need for nonurgent treatment: among lower-income individuals, having insurance slightly decreased the odds of needing nonurgent treatment, with this decrease in odds becoming greater for middle-income earners and even greater for high-income earners.
Conclusion: Income-related inequality in need for dental care exists even in the presence of dental insurance coverage and good dental hygiene habits. These findings highlight the need for increased access to dental care for low-income populations and families living in poverty.
Oral health problems, like other health problems, can limit a person’s activity, participation in the workforce, quality of life and mental health.1 Dental disease has been linked to chronic medical illnesses,2 as well as to functional, social and psychological limitations.3 Oral health is an essential aspect of general health; therefore, ensuring equity in oral health care is as important as ensuring equity in other forms of health care.
Income-related inequity in oral health has been well established both globally4 and in Canada,5-8 with higher levels of dental disease being concentrated among those with lower incomes and lower socio-economic status.9,10 In Canada, one mechanism for this socio-economic gradient may be the lack of publicly funded dental care. The majority of dental care costs are paid by Canadians either directly or through employer-provided or privately purchased insurance plans. The ability to pay for dental care or for insurance covering dental care is directly related to employment status, earnings and wealth.11 Although insurance coverage apparently increases access to dental care by reducing the direct costs of care, such coverage can be afforded only by those with sufficient disposable income to pay the premiums. It is therefore important to consider both income and dental insurance coverage when examining the effects of socio-economic disadvantage on oral health.
Previous Canadian studies have used data from the National Population Health Survey12 and the Canadian Community Health Survey13 to examine socio-economic gradients in dental care. Both of these studies found evidence of a gradient but were limited by how treatment need and dental care were measured. In addition, both studies relied on self-reported survey responses rather than direct assessments by dentists to evaluate dental care provided, and the data used for both studies are now at least 10 years old. Bhatti and colleagues13 admitted that their measure of use of dental services was “noisy,” in that it did not discriminate between different types and intensities of service use. In contrast, the current study used direct measures based on a dental examination, to allow for a more accurate measurement of the need for dental care.
Exploration of the effects of income and dental insurance coverage on the need for dental care is required to assess the extent of socio-economic inequities in dental care and to evaluate policy alternatives for addressing these inequities. To this end, confidential microdata from the 2009 Canadian Health Measures Survey were used to explore the effects of income and dental insurance coverage on the need for dental care. Potential variation in the effect of insurance coverage across income level was also examined.
Methods
This study was based on data from the 2009 Canadian Health Measures Survey, which was conducted from early 2007 to early 2009 with the aim of directly measuring key physical indicators that are relevant to the health of Canadians. The target population was Canadians aged 6 to 79 years, excluding institutional residents, full-time members of the Canadian Forces and people living on reserves or in Aboriginal settlements. The survey design drew on a subset of collection sites created for the area frame of Statistics Canada’s Labour Force Survey. Of the 257 sites created, a sample of 15 sites from Ontario, Quebec, British Columbia and Whitehorse, the Prairie provinces and the Atlantic provinces was selected for data collection. At each site, a stratified, random sample of 350 respondents was selected from a list of Census dwellings. A mobile clinic was set up at each collection site to provide a standard physical testing environment. After a household interview, each respondent was invited to the clinic, where a physical examination was conducted, and blood and urine samples were obtained. The oral health information used in the current study was derived from self-reported measures obtained in the household interviews and dentist-reported measures obtained during an oral examination conducted by a licensed dentist at the mobile clinic. Demographic information was collected during the household interview.
Of the overall sample of 5,604 respondents, 5,588 had dentist-completed information on need for treatment (data missing for 0.3%), and 4,874 had complete data for all variables of interest (income data missing for 6.7%, education data missing for 1.4%, immigration status missing for 0.5% and dental insurance information missing for 0.4%). Multiple imputation was used to impute missing data (SPSS software, version 19.0, IBM, Armonk, NY). All results shown here are pooled estimates from 5 imputed data sets. The final sample size was 5,604.
Dependent Variable
Need for Dental Care: Following an oral examination, the dentist recorded whether the participant required treatment to address any of the following issues: prevention, fillings, temporomandibular joint disorders, surgery, periodontics, esthetics, endodontics, orthodontics or soft tissue problems. The dentist was also asked to identify if the person required urgent treatment to address any of these concerns (except prevention and esthetics). From these data, a 3-category measure of need for dental care was created, coded as 0 = no treatment needed, 1 = nonurgent treatment needed (including esthetics and prevention) and 2 = urgent treatment needed.
Independent Variables
Household Income: Respondents were asked to estimate total household income. Additional questions were asked about the income category for each respondent. Statistics Canada then used these 2 variables (total income and income category) to create a 12-category household income variable. The midpoint of each category divided by 10,000 was used in the current analysis, such that a 1-unit increase in the income variable was equivalent to an increase in income of $10,000. This variable was centred to test for an interaction between income and dental insurance coverage. Centring refers to the process of subtracting the mean from all values so the mean of the variable is 0.
Dental Insurance Coverage: A dental insurance variable was created from the response to the question “Do you have insurance or a government program that covers all or part of your dental expenses?” The variable (coded as 1 = yes, 0 = no) was based on subjective recall; as such, some responses may have been incorrect among those without access to personal records.
The following demographic variables were used in the adjusted analyses: age (coded as 1 = 6–19 years, 0 =20–79 years; dichotomized because of the nonlinear relationship between age and need for dental treatment, with a significant increase in need for treatment after age 20 years), sex (coded as 1 = male, 0 = female), immigration status (born in Canada, immigrated less than 5 years ago or immigrated at least 5 years ago, with a distinction between recent and nonrecent immigrants because of expected differences in behaviour [5 years being the typical cut-off used to identify recent immigrants]), education (coded as 0 = graduated high school, 1 = less than high school) and province of residence (Quebec, British Columbia, New Brunswick, Alberta, Ontario). It should be noted that Statistics Canada recommends against conducting analyses at lower than the national level and sampling methods for the Canadian Health Measures Survey prevent representative comparisons between provinces. Nonetheless, province of residence was included as a control variable because of important provincial differences in socio-economic status and dental services, but the estimates must be interpreted with caution. In addition, 3 dental hygiene variables were used in adjusted analyses: brushing habits(coded as 0 = at least once a day, 1 = less than once a day), flossing habits (coded as 0 = at least once a week, 1 = less than once a week) and frequency of dentist visits(more than once a year, about once a year, less than once a year, only for emergencies, never). All variables except income were dichotomous or categorical, so dummy codes were created for the analysis.
Analysis
Multinomial logistic regression models were fitted to the data, and odds ratios and 95% confidence intervals (CIs) are reported. The logistic models predicted the probability of needing nonurgent or urgent dental care relative to those who did not need dental care. The analyses were performed and are reported sequentially. Model 1 was used to generate unadjusted estimates of the associations between household income (for which tests showed no nonlinearity) and dental insurance coverage and the need for dental care. Model 2 estimated these associations with adjustment for demographic characteristics, and model 3 controlled for both demographic characteristics and dental hygiene variables. SPSS 19.0 was used for all regression models. The analyses were weighted by the probability of selection, such that the results could be generalized to the overall population.
Results
Table 1 shows weighted characteristics for the whole sample (n = 5,604) and for the 3 subgroups: those needing urgent dental care (n =1,070), those needing nonurgent dental care (n =768) and those not needing any dental care (n =3,766). The percentage of participants with dental insurance coverage was lower among those needing dental care than among those who did not need care (55.1% and 63.5% vs. 72%); income was also lower among those needing care. The lowest level of insurance coverage was observed among those needing nonurgent care (55.1%). The percentages of males, of recent immigrants and of individuals aged 20 to 79 were higher among those needing dental care than among those not needing care. Among those needing dental care, higher percentages reported brushing their teeth less than once a day, flossing less than once a week and visiting the dentist less than once a year or only for emergencies, relative to those not needing care.
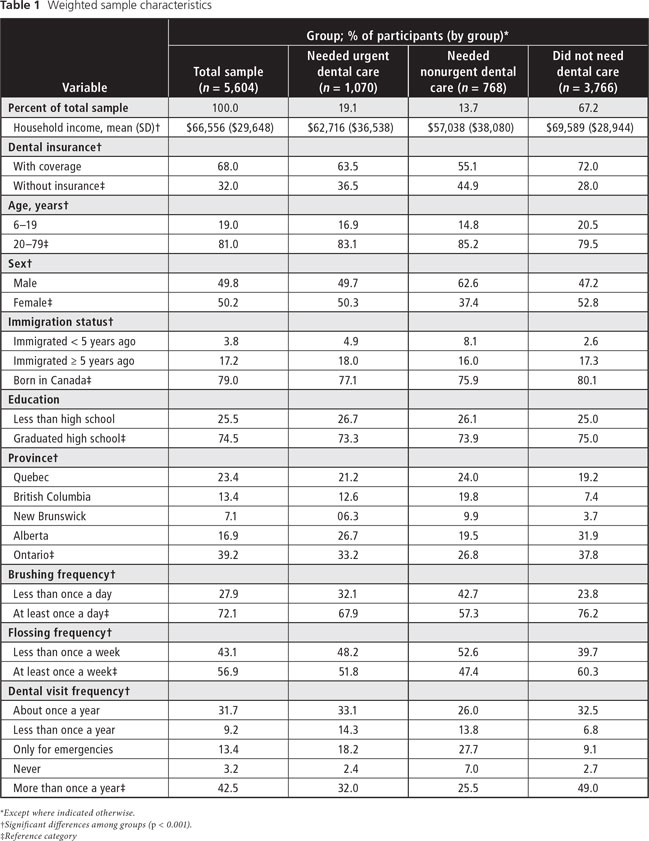
Table 2, based on the multinomial regression model 1, shows the unadjusted effects of dental insurance coverage and income on need for dental care. The odds ratio for insurance coverage was 0.59 for those needing nonurgent care and 0.76 for those needing urgent care. Therefore, relative to those with no need for treatment, the odds of needing nonurgent care were 41% lower for individuals with dental insurance coverage than for those without coverage. Similarly, the odds of needing urgent care were 24% lower for individuals with dental insurance than for those without coverage. The odds ratio for household income was 0.99 both for those needing urgent care and for those needing nonurgent care, which represents a 1% decrease in the odds of needing urgent or nonurgent dental care with each $10,000 increase in household income. The results for both insurance coverage and income were significant at the 0.001 level.
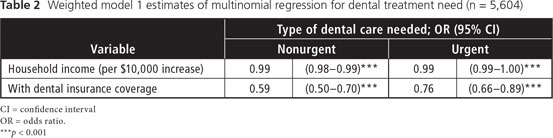
Table 3 shows the results for multinomial regression model 2, which controlled for demographic variables. The odds ratios for dental insurance coverage were slightly lower (0.58 for those needing nonurgent care and 0.69 for those needing urgent care) and the odds ratio for income remained the same (0.99) with these adjustments, and results for both insurance coverage and income remained statistically significant. The likelihood of needing nonurgent care was much higher for males than females and recent immigrants were much more likely to need urgent and nonurgent dental care compared to nonrecent immigrants and nonimmigrants.
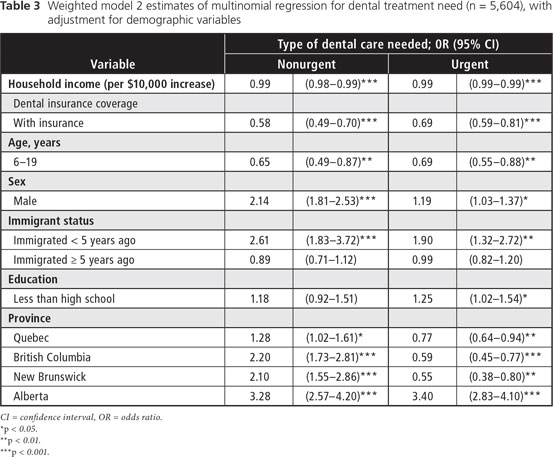
Table 4 shows results for multinomial regression model 3, which controlled for both demographic and oral health variables. Here, the odds ratios for dental insurance coverage declined toward the null value, representing a 20% reduction in the odds of needing urgent dental care and a 24% reduction in the odds of needing nonurgent dental care among individuals with dental insurance relative to those without insurance. The 0.99 odds ratio for household income remained statistically significant. The size of the significant effect for males decreased for those needing nonurgent care (relative to the result shown in Table 3). In addition, the effect for recent immigrants decreased for those needing nonurgent care and increased for those needing urgent care (relative to the results shown in Table 3).
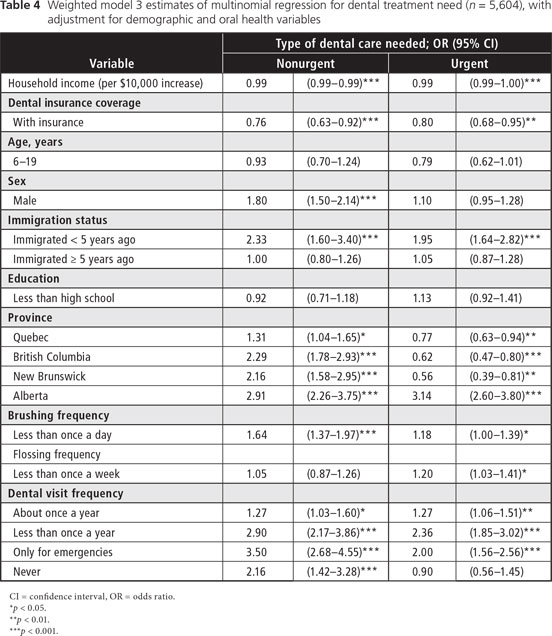
An interaction term between income and insurance coverage was added to model 3 and was significant for those needing nonurgent care (OR 0.99, p = 0.05); as such, having dental insurance moderated the relationship between income and odds of needing nonurgent care (Figure 1).
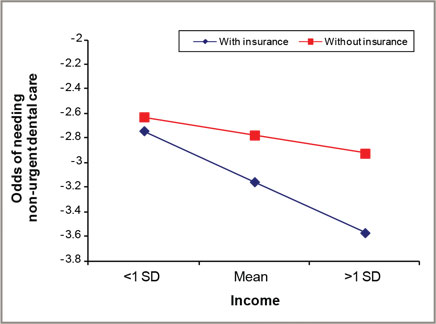 Figure 1: Association between income and odds of needing nonurgent dental care, with and without insurance. Having dental insurance coverage moderated this association.
Figure 1: Association between income and odds of needing nonurgent dental care, with and without insurance. Having dental insurance coverage moderated this association.
SD = standard deviation.
Discussion
Federal and provincial governments in Canada are committed to equitable health outcomes and to reducing health inequalities among Canadians. The findings presented here reveal significant income-related inequities in the need for both urgent and nonurgent dental care across Canada. These results are in accord with previous findings that the probability of receiving dental care is higher among individuals with higher levels of income and dental insurance coverage.12,13 Here, the effects of income were the same for both urgent and nonurgent treatment need relative to no treatment need. For those with dental insurance, the odds of needing nonurgent treatment were reduced by more than were the odds of needing urgent treatment (for nonurgent treatment need, 41% odds reduction with insurance; for urgent treatment need, 25% odds reduction with insurance), although the effect sizes were almost the same once demographic and dental hygiene variables were included (for nonurgent treatment need, 24% odds reduction with insurance; for urgent treatment need, 20% odds reduction with insurance). In this study, there was also a significant interaction between income and dental insurance with regard to need for nonurgent treatment. Although dental insurance can offer some assistance to low-income people for nonurgent dental care, the largest gains were realized by those with midlevel and higher incomes. Therefore, income-related inequality remained, even in the presence of dental insurance coverage.
As might have been expected, the model 3 results indicate that brushing, flossing and regular check-ups represent relatively low-cost steps that individuals can take to reduce the probability of needing urgent or nonurgent dental care. When these variables were included in the analysis, there was a decrease in the difference in need for dental care between those with and those without insurance. Maintaining a good dental hygiene regimen requires awareness of the positive effect of such practices, as well as the ability to make daily dental hygiene and the purchase of toothpaste, toothbrushes, floss and mouthwash a priority. However, doing so may be a challenge for low-income individuals and families living in poverty, who must also deal with food and financial insecurity. Nonetheless, including these preventive dental hygiene practices in the analysis did not decrease the income effect on dental care need, which indicates that the benefits of preventive care do not reduce the effects of socio-economic disadvantage.
These effects of socio-economic disadvantage on dental care are more far-reaching than whether a person can afford dental care. Low income and lack of insurance coverage are 2 manifestations of the effect that poverty has on health care equity. As a cause of poor diet, food insecurity, income inequality, and low levels of health literacy and education, poverty is the main challenge to dental health care equality.14-16 Only by addressing issues of poverty across Canada will it be possible to reduce socio-economic gradients in dental health care.
Although a number of oral health care initiatives are available to those living in poverty, it is recognized that these initiatives are not comprehensive and that they struggle to access funding.17,18 Finding a way to make dental care, including the more costly procedures, accessible to these individuals at relatively low cost presents a challenge to policy-makers. The Canadian Dental Association has advocated for publicly funded dental care for low-income individuals and an expansion of public health programs, but it has also recognized that such changes cannot be achieved without the collaboration of the dentistry profession, other health care professionals, charities, and the federal and provincial governments.19 The association has also called for the use of alternative models of care and the funding of a number of different solutions from providers in various settings. Future researchers might consider evaluating the effectiveness of these different care and funding models.
Given that socio-economic gradients exist across numerous aspects of health care, an attempt to integrate oral health care with general health care in terms of policy, funding and care provision could result in coordinated efforts in the fight against poverty. Such coordination might include provision of dental care within provincial public health programs that currently cover only some forms of dental surgery. Integrating service provision might mean that dental clinics for low-income families would operate 1 or 2 days a week at walk-in clinics or in general practitioners’ or family physicians’ offices. A broader approach might be the introduction of a peripatetic dental program for low-income families promoted by and provided at doctors’ offices, schools and other health or community centres in particularly vulnerable areas. Monitoring and evaluation to determine the efficiency and effectiveness of any such strategy will be key until the issue of poverty is more fully addressed.
Conclusions
This study examined the effects of income and dental insurance coverage on need for dental care and found evidence of socio-economic gradients in the need for both urgent and nonurgent dental care. The observed associations confirmed previous findings and showed that these inequalities have persisted over time. The results have also shown that income-related inequities exist even in the presence of dental insurance coverage and good dental hygiene practices. This evidence suggests that low income and poverty are the main issues in dental health care inequality. Addressing health-related socio-economic inequities is certainly a challenge but must be done if Canada is to fulfill its commitment to equitable health outcomes for all its citizens.
THE AUTHORS
References
- Gift HC, Atchison KA. Oral health, health, and health-related quality of life. Med Care. 1995;33(11 Suppl):NS57-72.
- Cooney P. Preface to the Canadian Health Measures Survey results – oral health statistics, 2007-2009. Chronic Diseases in Canada. 2010;30(4):115-6.
- Locker D, Matear D. Oral disorders, systemic health, well being and the quality of life - A summary of recent research evidence. Community Health Services Research Unit, Faculty of Dentistry, University of Toronto. [Accessed 2014 Jan 28]. Available: http://s3.amazonaws.com/zanran_storage/www.utoronto.ca/ContentPages/9519770.pdf
- Hosseinpoor AR, Itani L, Petersen PE. Socio-economic inequality in oral healthcare coverage: results from the World Health Survey. J Dent Res. 2012;91(3):275-81.
- Grignon M, Hurley J, Wang L, Allin S. Inequity in a market-based health system: Evidence from Canada’s dental sector. Health Policy. 2010;98(1):81-90.
- Locker D. Deprivation and oral health: a review. Community Dent Oral Epidemiol. 2000;28(3):161-9.
- Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 2007;35(1):1-11.
- Main P, Leake J, Burman D. Oral health care in Canada – a view from the trenches. J Can Dent Assoc. 2004;72(4):319a-319f.
- Snow P, McNally ME. Examining the implications of dental treatment costs for low-income families. J Can Dent Assoc. 2010;76(2):a28.
- Sabbah W, Tsakos G, Chandola T, Sheiham A, Watt RG. Social gradients in oral and general health. J Dent Res. 2007;86(10):992-6.
- Muirhead VE, Quinonez C, Figueiredo R, Locker D. Predictors of dental care utilization among working poor Canadians. Community Dent Oral Epidemiol 2009;37(3):199-208.
- Millar W, Locker D. Dental insurance and use of dental services. Health Rep. 1999;11(1):55-67 (Eng); 59-72(Fre).
- Bhatti T, Rana Z, Grootendorst P. Dental insurance, income and the use of dental care in Canada. J Can Dent Assoc. 2007;73(1):57.
- Bhaatacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23(4):839-62.
- Evans GW. The environment of childhood poverty. Am Psychol. 2004;59(2):77-92.
- Aber JL, Bennett NG, Conley DC, Li J. The effects of poverty on child health and development. Annu Rev Public Health. 1997;18:463-83.
- Wallace BB, MacEntee MI. Access to dental care for low-income adults: Perceptions of affordability, availability and acceptability. J Community Health. 2012;37(1):32-9.
- Canadian Dental Association. Position Paper on Access to Oral Health Care for Canadians. 2010. [Accessed 2012 Mar 12]. Available: http://www.cda-adc.ca/en/about/media_room/position_statements/
- Muirhead V, Quinonez C, Figueirdo R, Locker D. Oral health disparities and food insecurity in working poor Canadians. Community Dent Oral Epidemiol. 2009;37(4):294-304.


