Anesthesia services are an important consideration in dental care from both the patient’s and the clinician’s perspective. This paper discusses anaesthesia services with respect to deep sedation and general anaesthesia (GA). The American Dental Association (ADA) defines deep sedation as “a drug-induced depression of consciousness during which patients cannot be easily aroused but respond purposefully following repeated or painful stimulation, with the ability to independently maintain ventilator function being potentially impaired.”1 The ADA further define general anaesthesia (GA) as “a drug-induced depression of consciousness during which patients are not arousable, even by painful stimulation, with the ability to independently maintain ventilator function being often impaired.” 1 Anaesthesia services benefit patients who would otherwise not have dental treatment because of fear,2-7 treatment complexity, medical conditions, behavioural challenges or a pronounced gag reflex.4,8-11 The use of anesthesia has a positive impact on patients’ oral health by increasing attendance for treatment.2,12-14 As with all procedures, the decision to use sedation or GA is based on full consideration of the relative benefits and risks. Dental patients are not always aware of the choices they may have with regard to anesthesia services;2,14 however, when asked, patients in Canada and other parts of the world report an interest in, and preference for, sedation or GA in conjunction with dental treatment.2,3,7-10 Little is known about dentists’ views and their use of sedation and anesthesia in clinical practice,9,15,16 whether they are aware of their patients’ preference for these services or whether they provide them as often as patients would like.
Although only one of many factors, dental anxiety has a major influence on a patient’s choice of sedation and GA.2,8,12,14,17-20 Self-reporting is commonly used to determine patient anxiety; however, patients are not always willing to discuss or acknowledge their dental anxiety. Consequently, clinicians often assess patient anxiety independent of patient input. As fearful patients may prefer sedation and GA, interest lies in dentists’ ability to estimate patient anxiety, as this may influence their perception of patient interest in sedation and GA services and their likelihood of offering such services to patients during their dental treatment.
This article is part of a larger study related to dentists’ views and use of sedation and GA in Ontario. The purpose of this paper is to report dentists’ perceptions of patient interest in sedation and GA and their estimation of patient fear and avoidance of dental care. Data from this study were compared with previously reported patient findings8 to examine possible differences between dentist and patient views.
Methods
Dentist selection
Dentists were selected from the Royal College of Dental Surgeons of Ontario (RCDSO) roster of 8670 licensed dentists in Ontario in 2011. To be included, dentists had to be practising and have an email address in their RCDSO contact information. This reduced the possible number of participants to 6613. We randomly selected 3001 dentists to ensure a sufficient sample size of 600 based on an expected 20% response rate, 95% confidence interval and 4% sampling error.21
Ethics approval (#26860) was received for this study from the Health Sciences 1 Ethics Review Board at the University of Toronto.
Data collection
This descriptive study incorporated a cross-sectional survey method, with data collected over 6 weeks. To maximize response rate, clinicians were contacted 4 times.21 The first contact was a mailed package sent to all dentists in our sample; it included an invitation to participate and a paper copy of the survey with a stamped return-addressed envelope. The second contact, an email invitation to complete the survey online, was sent to non-responders. The third contact, by email, was to thank respondents for participation, and to remind non-responders to complete the survey. A final email invitation to participate was sent to all non-responders 48 hours before study closing.
Survey
The survey comprised 16 questions designed to assess dentists’ views on sedation and their practice patterns. The questions were modified from similar ones asked of Canadian adults in a 2002 telephone survey 8 regarding their interest in sedation for dental treatment, level of dental fear and avoidance of dental care. Demographic data was also collected, including dentists’ sex, years in practice, type of practice and size of community served.
The survey was field tested in a sample of general and specialist dentists (n = 20) to assess face validity, comprehension, and clarity, with revisions made based on comments received.
Data analysis
SPSS version 20 was used for descriptive and inferential statistical analysis. Mixed-design analysis of variance (ANOVA) assessed demographic variables and responses. If a main effect or an interaction was found to be statistically significant, ANOVA was followed by independent sample t-tests and 1-way ANOVA. Dentists’ estimates and patients’ self-reported findings were analyzed using 1-sample t-tests. Patient self-reported data from a 2002 survey served as reference values.8 All tests were interpreted with α = 0.05 as the criterion for statistical significance.
Results
Responses were received from 1076 dentists (713 by mail; 363 online) representing a 37.9% response rate.
Study participants were 69.7% male and 30.3% female. General practitioners comprised 84.4% of the sample, with the remaining 15.6% representing clinicians from all 10 dental specialties in Ontario (Table 1). Years of practice ranged from 0.5 to 42.0, with a mean of 20.6 years. We divided these data into thirds: ≤ 13 years, 13.1–27.0 years and > 27 years of practice. Regarding size of community served, 42.2% of participants had their primary practice in a city with a population over 500,000; 39.1% were in cities with 50,000–500,000 inhabitants; and 18.7% were in towns with fewer than 50,000 inhabitants. Using the RCDSO database, we confirmed that the study population was representative of practising dentists in Ontario with respect to surveyed demographic variables.
| Characteristic | N (%) |
|---|---|
| Sex (n = 1036) | |
| Male | 722 (69.7) |
| Female | 314 (30.3) |
| Practice type (n = 1036) | |
| General practitioner | 874 (84.4) |
| Dental anesthesiologist | 9 (0.9) |
| Dental public health specialist | 8 (0.8) |
| Endodontist | 22 (2.1) |
| Oral medicine/oral pathologist | 4 (0.4) |
| Oral and maxillofacial radiologist | 1 (0.1) |
| Oral and maxillofacial surgeon | 22 (2.1) |
| Orthodontist | 23 (2.2) |
| Pediatric dentist | 25 (2.4) |
| Periodontist | 25 (2.4) |
| Prosthodontist | 23 (2.2) |
| Years in clinical practice (n = 1034; mean: 20.6 years) | |
| ≤ 13.0 | 346 (33.5) |
| 13.1–27.0 | 366 (35.4) |
| > 27.0 | 322 (31.1) |
| Community size (n = 1035) | |
| ≤ 50,000 | 193 (18.6) |
| 50,001–500,000 | 405 (39.1) |
| > 500,000 | 437 (42.2) |
Dentists’ views of patient interest in sedation and general anesthesia
When asked whether they thought patients were interested in sedation and GA, dentists reported that two thirds (66.8%) of patients were “Not interested” whereas the majority of patients (55.7%) answering the 2002 survey were “Interested depending on cost” or “Definitely interested” (Fig. 1). Dentists also predicted that only 19.8% of patients would be “Interested depending on cost” compared with a much higher proportion (42.3%) of patients (p < 0.01). However, dentists and patients were similar in their estimates of patients who are “Definitely interested” in sedation and GA, at 13.4% and 13.5%, respectively.
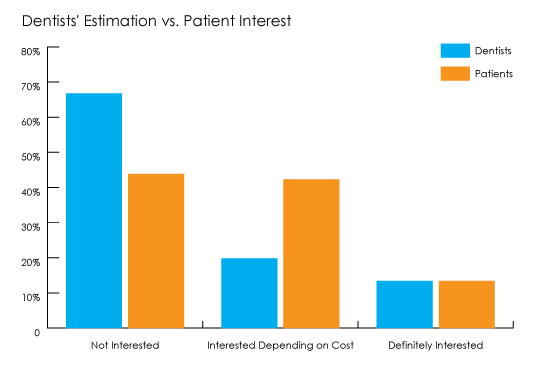 *Significant difference between dentists and patients (p < 0.01).
*Significant difference between dentists and patients (p < 0.01).Dentists’ estimate of patient interest in sedation and GA varied with sex, years of experience, and size of the community they served (Table 2). Dentists with 13 years of clinical experience or less reported significantly different perceptions of patient interest in sedation and GA compared to those with more experience for all interest categories (p < 0.01). Male and female dentists differed with respect to “Interest depending on cost”, with male dentists reporting patients being less interested compared to their female counterparts (p < 0.01). The size of the community in which the dentist practised did not affect their estimation of patient interest in sedation and GA.
| Dentist category | Dentists’ perception of patients’ interest in sedation (%) | ||
|---|---|---|---|
| Not interested | Interested depending on cost | Definitely interested | |
| Note: In each group, values followed by the same letter are significantly different at the p < 0.01 level. | |||
| Sex (n = 1036) | |||
| Male | 67.4 | 18.7a | 13.1 |
| Female | 64.6 | 23.2a | 12.2 |
| Years of experience (n = 1034) | |||
| ≤ 13.0 | 58. 7ab | 24.8ab | 16.5ab |
| 13.1–27.0 | 70.0b | 18.3b | 11.7b |
| > 27.0 | 71.6a | 16.4a | 11.9a |
| Community size (n = 1035) | |||
| ≤ 50,000 | 67.4 | 20.3 | 12.3 |
| 50,001–500,000 | 64.2 | 21.2 | 14.6 |
| > 500,000 | 68.5 | 18.7 | 12.8 |
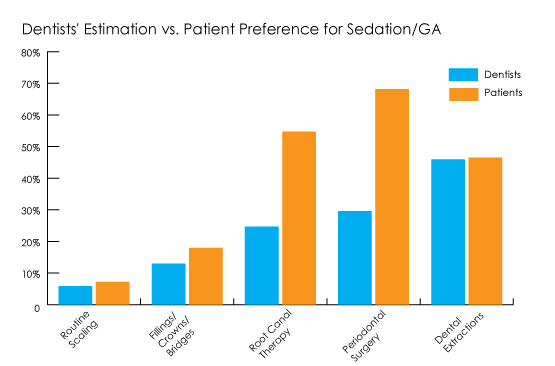
Dentists were also asked to estimate their patients’ preference for anesthesia services for a variety of procedures, including routine scaling; fillings, crowns and bridges; root-canal therapy; periodontal surgery; and extractions (Fig. 2). Dentists underestimated patient preference for sedation and GA for all procedures (p < 0.01), except extractions where no difference was noted between groups. The largest differences between dentists and patients were reported for root-canal therapy (24.7% v. 54.7%, respectively) and periodontal surgery (29.6% v. 68.2%, respectively). As well, dentists estimated patient interest in sedation and GA to be greatest for extractions whereas patients indicated greatest preference for anesthesia for periodontal surgery followed by root-canal therapy.
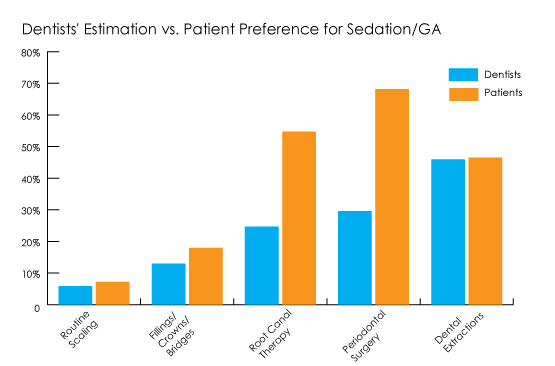 *Significant difference between dentists and patients (p < 0.01).
*Significant difference between dentists and patients (p < 0.01).
Dentists with less than 13 years of experience reported significantly higher estimates of patient interest in sedation and GA for fillings, crowns and bridges; root-canal therapy; periodontal surgery; and dental extractions than their more experienced colleagues (p < 0.01); however, their estimates were still significantly lower than those of patients (p < 0.01), except for extractions. No differences based on sex or size of the community in which they practise were noted in dentists’ estimates of patients’ desire for sedation for the various procedures (Table 3).
Dentists’ estimation of patient fear and avoidance of dental treatment
Dentists’ perception of patients’ fear was significantly higher (p < 0.01) than patients’ reports for all fear categories (Fig. 3). The largest differences were in dentists’ estimates of patients who were “Not afraid” (38.6% compared with patient reports of 63.9%) or “Very afraid/terrified” (16.6% v. 5.5%). Dentists with less experience (≤ 13 years) also estimated significantly higher levels of fear in patients than experienced dentists. They perceived that 19.9% of patients are “Very afraid” or “Terrified” compared with more experienced dentists who reported 14.6% and 14.2% of patients with those levels of fear (p < 0.01) (Table 4). With respect to sex, female dentists estimated more patients as “Somewhat afraid” compared with male clinicians (22.4 % v. 18.7%) (p < 0.01). A difference was noted based on community size, with dentists in communities of under 50,000 people estimating that more patients are a “Little afraid” than practitioners in larger cities (p < 0.01).
Dentists also believed that more patients avoid dental appointments because of fear or anxiety (13.3%) than patients reported (7.6%) (p < 0.01), with female dentists’ estimates of the percentage of patients avoiding a dentist being significantly higher than male practitioners (16.0% v. 12.9%; p < 0.01). Similar to the fear data, dentists who were ≤ 13 years in practice estimated that more patients miss, cancel or avoid dental appointments than dentists with > 27.0 years of experience (p < 0.01). No significant difference was reported based on the size of the community in which the dentist practised.
| Dentist category | Dentists’ perception of patients’ interest in sedation (%) | ||||
|---|---|---|---|---|---|
| Routine scaling | Fillings, crowns, bridges | Root canal therapy | Periodontal surgery | Dental extraction | |
| Note: In each group, values followed by the same letter are significantly different at the p < 0.01 level. | |||||
| Sex (n = 1036) | |||||
| Male | 5.9 | 13.0 | 24.2 | 29.1 | 44.1 |
| Female | 5.6 | 12.5 | 25.1 | 27.1 | 48.5 |
| Years of experience (n=1034) | |||||
| ≤ 13.0 | 6.3 | 14.1a | 27.0ab | 31.5a | 49.4ab |
| 13.1–27.0 | 5.4 | 11.1ab | 23.1a | 25.0ab | 43.7b |
| > 27.0 | 5.8 | 13.5b | 23.0b | 29.3b | 42.8a |
| Community size (n = 1035) | |||||
| ≤ 50,000 | 5.5 | 13.0 | 24.0 | 28.3 | 44.5 |
| 50,001–500,000 | 5.9 | 13.2 | 25.4 | 29.0 | 46.3 |
| > 500,000 | 5.8 | 12.3 | 23.6 | 28.0 | 45.0 |
| Dentist category | Dentists’ perception of level of patients’ fear (%) | |||||
|---|---|---|---|---|---|---|
| Not afraid | Little afraid | Somewhat afraid | Very afraid | Terrified | ||
| Note: In each group, values followed by the same letter are significantly different at the p < 0.01 level. | ||||||
| Sex (n = 1036) |
||||||
| Male | 39.6 | 25.7 | 18.7a | 10.1 | 5.8 | |
| Female | 36.5 | 23.1 | 22.4a | 11.2 | 6.3 | |
| Years of experience (n = 1034) |
||||||
| ≤ 13.0 | 34.9ab | 24.3 | 21.0 | 12.8ab | 7.2ab | |
| 13.1–27.0 | 40.7b | 25.1 | 18.6 | 9.2b | 5.4b | |
| > 27.0 | 40.2a | 25.3 | 19.8 | 9.2a | 5.0a | |
| Community size (n = 1035) |
||||||
| ≤ 50,000 | 35.5 | 29.0ab | 20.0 | 10.1 | 5.6 | |
| 50,001–500,000 | 38.4 | 24.4b | 20.1 | 10.6 | 6.3 | |
| > 500,000 | 40.2 | 23.6a | 19.4 | 10.4 | 5.7 | |
Discussion
Patient interest in sedation and general anesthesia
A significant difference was noted between dentists’ perception of patients’ interest and patients’ reported interest in sedation and GA for dentistry. The disparity might be explained in part by practitioner views, including a belief that cost prohibits patients from accepting sedation and GA,9,20 that patients believe sedation and GA to be unsafe,8,16 or that local anesthesia is adequate for most dental treatments.16 No guidelines currently exist to help dentists assess which patients would benefit from sedation services.
Sedation and GA are used commonly in the medical community for treatments ranging from elective preventive procedures, such as endoscopy, to life-saving surgery. However, patients may not know the anesthesia options available with respect to dental treatment.19 It is unknown whether dentists routinely offer anesthesia services to all patients irrespective of procedure or patient fear. Studies in Sweden and the United Kingdom attribute an increased use of anesthesia to greater patient awareness of sedation services.13,22 Notably, United Kingdom researchers reported 38% of surveyed patients were unaware of the availability of sedation and GA options in dentistry.2 The percentage of patients aware of dental anesthesia options and the associated costs is not known for Canada. However, if Ontario patients in 2011 were more knowledgeable of anesthesia options in dentistry than the Canadian patients surveyed in 2002,8 a higher percentage of patient interest in sedation and GA may be expected, resulting in an even greater discrepancy between the views of dentists and patients today than reported in this study.
This study also noted that dentists underestimate patients’ preference for sedation and GA for all types of dental procedures, except extractions. Anesthesia costs for this treatment may be inconsequential to practitioners and patients, as many dental insurers cover anesthesia fees in conjunction with extractions.23 Furthermore, the use of sedation and GA for extractions may be entrenched among both patients and dentists, who may intuitively recognize this procedure as invasive or associated with patient anxiety. In contrast, dentists underappreciated patient preference for sedation and GA during root-canal therapy and periodontal surgery, procedures for which clinicians may not typically use sedation and GA or may not receive dental insurance reimbursement. Furthermore, patients may perceive root-canal therapy and periodontal surgery to be more invasive than clinicians do and, therefore, to warrant sedation.8,13
Dentists’ estimation of patient levels of fear and avoidance of dentistry
Dental fear in patients is well documented 2,7,8,12,17,18 and can motivate anxious patients to choose sedation and GA for dentistry. 2,6-8,14,19,24 Furthermore, anxiety toward dentistry may manifest as avoidance of services 2,12,14,19,20 and, subsequently, untreated dental disease.5-7 As a result, it is important for the practitioner to identify and manage patient anxiety to enhance attendance at appointments and dental care.10,14,17 In this study, Ontario dentists overestimated patient-reported anxiety and avoidance of dental treatment. The significant difference between dentists’ and patients’ perceptions with respect to fear reinforces the fact that dental anxiety is a complicated phenomenon to assess.3,8,19,25 Numerous factors create great variation among dentally anxious people,3 and fear can be magnified or potentiated in even the mildly anxious depending on the clinical context.2,26 Such complexity can affect dentists’ ability to identify dentally fearful patients consistently and correctly. An alternative hypothesis is that patients under-report their own anxiety, which is detected by their dentist.
The literature is limited in terms of the methods practitioners use to assess anxiety. An Irish study reported that 14% of dentists assess anxiety in some formal manner; however, only 2% use a validated questionnaire.17 It is unknown whether dentists choose not to use formal scales or prefer to rely on their perception of their patients’ anxiety.
Overall, this study highlights the disconnect between patient and practitioner views of patients’ fear and avoidance of dental services and their preference for sedation and GA. Although practitioners estimated greater fear and avoidance of dental care than patients reported, dentists underestimated patient preference for sedation and GA, a clinically suitable method to manage patient anxiety.2,6-8,14,19,24 Even if we assume clinicians are correct and patients are more fearful than they admit, it is notable that dentists did not identify a corresponding preference for sedation and GA.
Effect of sex, clinical experience and community size on dentists’ perceptions
Significant differences in estimating patient preference for sedation and GA, patient anxiety and dental avoidance were reported between male and female practitioners, and based on years of experience. Such findings deserve further research to determine the clinical impact these variables have on dentists’ perceptions of sedation and GA use in dentistry.
Study strengths and limitations
The main strength of this study is the comparison between dentists’ perceptions of patient beliefs and patient data regarding sedation and GA. The response rate was higher than expected, and survey participants were representative of Ontario dentists in terms of sex, mix of generalists and specialists, clinical years of experience and size of the community of practice. This confers some confidence that the data reported may be generalized to reflect beliefs of dentists across the province.
A limitation of the study is the time and geographic differences between the provincial dentist survey and the national patient survey. Patient awareness of sedation and GA and economics may have changed in the 9 intervening years; however, no Canadian patient surveys have been conducted since 2002 to determine whether any difference exists. Consistent with our results; however, studies among patients in other countries show preference for sedation and GA rates considerably higher than Ontario dentists estimated in 2011.17,24 Finally, with no access to the original patient data including standard error information, we were limited in making statistical comparisons.
Conclusion
This study identifies significant differences between the views of dentists and patients with respect to patient interest in sedation and GA, as well as patient fear and avoidance of dental care. Dentists need to recognize that patients are interested in sedation and GA for procedures other than extractions. These discrepancies may affect the availability and provision of sedation and GA in Ontario.





